 Familial Hypercholesterolemia and Statin Drugs
Familial Hypercholesterolemia and Statin Drugs
by Jeffrey Dach MD
Left image: Red arrows: Heavily calcified coronary artery on CAT Scan.
A Major Dogma of Mainstream Medicine
One of the major dogmas of mainstream medicine is the miraculous benefit of statin drugs in the battle against atherosclerotic heart disease. I have written a number of previous articles which review the medical studies on this showing that statin drugs actually do have justifiable use in certain segments of the population, namely middle aged men with known heart disease. However, statin drugs are not justified in women, the elderly or in the primary prevention setting. This is true because in women, the elderly and in the primary prevention there is no mortality benefit to outweigh the adverse effects.
Familial Hypercholesterolemia- Higher Risk of Heart Disease
 How about the sub-group of the population with a genetic mutation called familial hypercholesterolemia, in which the serum cholesterol is markedly elevated because of a mutation in the LDL receptor? This is a common mutation affecting one in five hundred people.(1)
How about the sub-group of the population with a genetic mutation called familial hypercholesterolemia, in which the serum cholesterol is markedly elevated because of a mutation in the LDL receptor? This is a common mutation affecting one in five hundred people.(1)
Left Image: Normal Coronary Artery with No Calcification (Red Arrows) CAT Scan.
Mainstream medicine says that this genetic trait, familial elevated cholesterol (usually above 300), carries a higher risk for atherosclerotic heart disease, and increased mortality at a young age. In the heterozygous condition, the risk of a “coronary event” by the age of 60 years without treatment is about 50% in men and 30% in women.(1) Surely, if statins drugs have any utility, it must be for this group of people with elevated cholesterol due to a genetic disease.
Case Report- A Woman With Multiple Thyroid Nodules on Statin Drugs
Ann, a 61 year old real estate agent and grandmother came to see me in the office because of a number of tiny thyroid nodules which had been previously biopsied showing an indeterminate result. They couldn’t decide if it was benign or malignant, so her doctors recommended thyroid surgery with total thyroidectomy, “just to be sure”.
Thinking this a bit hasty, Anne came to see me for a second opinion. I explained to Anne multiple tiny thyroid nodules were quite common in the population, most likely of no clinical significance. My previous article, The Thyroid Nodule Epidemic , discussed this. I suggested we follow the nodules with serial ultrasound studies while providing medical treatment to shrink the nodules.
Statin Drug for High Cholesterol
In addition, Anne had been taking a statin drug for high cholesterol and had obvious adverse drug effects of muscle weakness, muscle pain and memory loss.
Anne’s lab panel showed a cholesterol of 240 which I consider faily normal for women. My usual approach in this scenario is to suggest a Coronary Calcium Scan to assess the amount of underlying arterial plaque and to answer the question, “Does Anne need statin drugs”?
Anne’s calcium score test result came back “Zero”, meaning her arteries are clean with no significant blockage, and there is no need for a statin drug to prevent heart disease, as there was nothing there to prevent.
One Year Later
 One year later, Anne was relieved and happy to learn the follow-up ultrasound scan showed the thyroid nodules were smaller in size, indicating that Anne certainly did not need thyroid surgery.
One year later, Anne was relieved and happy to learn the follow-up ultrasound scan showed the thyroid nodules were smaller in size, indicating that Anne certainly did not need thyroid surgery.
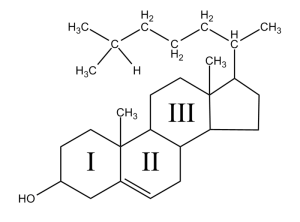
Also at this same one year follow up visit, a repeat cholesterol lab panel showed that Anne’s cholesterol, off the statin drug, had gone up to 330. The cholesterol had previously been 241 while taking a statin drug. Above left image: chemical structure of cholesterol courtesy of wikimedia commons
It Has Always Been Elevated
I then asked Anne if her cholesterol had ever been elevated in the past, and she said yes, it has always been elevated in the 300’s her whole life. Not only that, her parents both have high cholesterol (in the 300’s), and her sisters and brother also have the same thing. After hearing this, in one of these “Aha moments”, I said to Anne, “you must have familial hypercholesterolemia !”
Statin Drugs for Familial Hypercholesterolemia (FHC)
This complicates the issue. Indeed, Anne’s mainstream medical doctor has been giving Anne a statin drug for the past 10 years to lower her cholesterol from 330 to 240. In spite of the “Zero” calcium score, should Anne be taking a statin drug because of the familial hypercholesterolemia (FHC), a risk factor for heart disease ?
 Simon Broome Familial Hyperlipidaemia Registry in the UK
Simon Broome Familial Hyperlipidaemia Registry in the UK
The answer comes from a 2008 study from the Simon Broome Familial Hyperlipidaemia Registry in the United Kingdom.(1,2)
Left Image: Satellite Photo of the UK, United Kingdom courtesy of wikimedia commons.
In this study, Three Thousand Four hundred (3400) patients with familial hypercholesterolemia (FHC) were recruited from 21 clinics in the UK and followed for 26 years (46,580 person-years).(1) What did they find? Here is a quote from the study:
“Familial hypercholesterolaemia is associated with a substantial excess mortality from coronary heart disease in young adults but may not be associated with a substantial excess mortality in older patients. “(2)
Mortality Depends on Age
The authors looked at data both before and after the availability of statin drugs.
“Before statin drugs were available, mortality from coronary disease was increased nearly 100-fold in young adults with FHC aged 20–39 years, and increased about 4-fold for patients aged 40–59 years, but in those surviving through middle age, risk was similar to the general population.” (1)
In other words, if a patient survives past 60 with no heart disease, then they are no longer at increased risk. They have the same risk as the general population.
“Both before and after statins became widely available, there was no excess coronary mortality in patients aged >60 years without known coronary disease. Patients surviving into older age before statins became available were therefore likely to be a highly selected group at lower risk of coronary disease.”(1)
A Highly Selected Group at Lower Risk of Coronary Disease
The Simon Broome Registry of FHC answers our question.(1,2) At age 61, Anne still has no history of heart disease, and indeed her calcium score of zero indicated no plaque and no heart disease. Therefore, Anne must be a member of a “highly selected group at lower risk of coronary disease”.
If Anne’s high cholesterol over a lifetime placed her at risk, surely she would have developed some evidence of heart disease by now. The fact that her calcium score is low means that Anne is at low risk for heart disease. For Anne, adding a statin drug to prevent heart disease is not necessary and ill advised, since Anne is not at risk. Statin drugs carry significant adverse effects with reduced memory and cognitive function, muscle pain, neuropathy etc.
An Argument Against the Cholesterol Theory of Heart Disease
Think about it. Thousands of people with familial hypercholesterolemia who have elevated cholesterol above 330-350 for their entire lives, reach the age of 60 years, and never develop heart disease. This is one of the strongest arguments against the theory that cholesterol causes heart disease.
Reduce Cholesterol Naturally
The Simon Broome Registry study was re-assuring. Anne felt comfortable avoiding the statin drugs, and instead use Bergamot, a citrus food supplement called CholestePurePlus.(3,4) Studies show a 25-30% reduction in cholesterol with Bergamot without adverse side effects associated with statin drugs.(4)
In addition, we plan to follow Anne’s calcium score with an annual Coronary Calcium Score. Should Anne’s calcium score increase, indicating more plaque formation, then a more aggressive form of intervention would be justified.
Articles with Related Interest
Heart Disease Vitamin C and Linus Pauling
Getting Off Statin Drug Stories
How to Reverse Heart Disease with the Coronary Calcium Score
Cholesterol Lowering Drugs for the Elderly, Bad Idea
Cholesterol Lowering Statin Drugs for Women Just Say No
Reductions in all-cause, cancer, and coronary mortality in statin-treated patients with heterozygous familial hypercholesterolaemia: a prospective registry study.
Neil A, Cooper J, Betteridge J, Capps N, McDowell I, Durrington P, Seed M, Humphries SE.Source NIHR School of Primary Care Research, Division Public Health and Primary Health Care, University of Oxford, Old Road Headington, Oxford, UK.
Methods and results A total of 3382 patients (1650 men) aged <80 years were recruited from 21 lipid clinics in the United Kingdom and followed prospectively between 1980 and 2006 for 46 580 person-years. There were 370 deaths, including 190 from coronary heart disease (CHD) and 90 from cancer. The standardized mortality ratio (compared with the population in England and Wales) was calculated before and from 1 January 1992. In patients aged 20–79 years, CHD mortality fell significantly by 37% (95% CI = 7–56) from 3.4- to 2.1-fold excess. Primary prevention resulted in a 48% reduction in CHD mortality from 2.0-fold excess to none, with a smaller reduction of nearly 25% in patients with established disease. Coronary mortality was reduced more in women than in men. In patients without known CHD at registration, all-cause mortality from 1992 was 33% (21–43), lower than in the general population, mainly due to a 37% (21–50) lower risk of fatal cancer.Introduction
Familial hypercholesterolaemia (FH) is an autosomal co-dominant disorder.1 Defects in at least three different genes that code for proteins involved in hepatic clearance of low-density lipoprotein-cholesterol (LDL-C) can cause FH. These include, most commonly, mutations in the gene coding for the LDL-receptor that removes LDL,2 much less commonly in the gene for Apolipoprotein B which is the major protein of the LDL particle, and rarely in the gene coding for an enzyme called PCSK9 involved in degrading the LDL receptor.3 In all cases, this results in an accumulation of LDL in the plasma from birth, and to subsequent development of tendon xanthomas, xanthelasmas, and atheroma.1
The aim of this paper was to extend our previous reports7,10–13 by studying an enlarged cohort of 3382 heterozygous patients followed for up to 26 years until the end of 2006, by when the exposure had more than doubled to 46 580 person-years. This has allowed us to examine more informatively the changes in mortality compared with the general population both before and after the routine use of statins.Principal findings : This large long-term prospective registry study of 3382 patients with heterozygous familial hypercholesterolaemia demonstrates a statistically significant reduction in coronary mortality of about one-third since the widespread use of statins.
2) http://www.ncbi.nlm.nih.gov/
BMJ. 1991 October 12; 303(6807): 893–896.
Risk of fatal coronary heart disease in familial hypercholesterolaemia. Scientific Steering Committee on behalf of the Simon Broome Register Group.
——————————
bergamot study Bergamot PolyphenolsThe Bergamot orange (Citrus bergamia) is a yellow-colored citrus fruit the size of a lemon mainly grown in the southern Calabria region of Italy. It is distinct from other citrus fruits based on its unique profile and high concentration of flavonoids and flavonoid glycosides. Preliminary cell-based and animal research studies have shown several of these flavonoids to possess anti-atherosclerotic properties, including the ability to inhibit LDL oxidation. Some also have structural similarity to the natural substrate of the HMG-CoA reductase enzyme, which is the major target of statin drugs. Inhibiting this enzyme’s function serves to decrease cholesterol synthesis.
A recent study by Vincenzo Mollace and colleagues in Italy (Fitoterapia, 2011) investigated the effect of bergamot extract high in polyphenols, in both rats and humans. In rats with diet-induced hyperlipidemia, 10 and 20 mg/kg of bergamot polyphenols orally administered daily for 30 days led to significant reductions in total cholesterol, LDL, and triglycerides, with moderate elevations in HDL cholesterol levels seen compared to rats fed the hypercholesterolemic diet alone.
The human study was conducted as a randomized, double-blind, placebo-controlled trial consisting of 237 patients with high cholesterol levels (104 patients with isolated hypercholesterolemia/LDL levels greater than 130 mg/dL) (Group A); 42 patients with elevated cholesterol and triglycerides (Group B); 59 patients with high cholesterol, triglycerides, and blood sugar (Group C); and a final group of 32 patients classified as post–statin therapy who had stopped simvastatin due to musculoskeletal and liver adverse effects (Group D). Each of the above groups was divided into three subgroups. One subgroup received 500 mg of bergamot polyphenols per day; the second received 1000 mg/day; the third group received placebo. The post–statin therapy group received 1500 mg of bergamot polyphenols per day after a 60-day statin washout period. All patients were treated for 30 days.
In aggregate, groups A, B, and C showed an average reduction in total cholesterol of 21.8% and LDL cholesterol of 24.1% and an increase in HDL levels of 22.3% with 500 mg/day. The group taking 1000 mg/day of bergamot polyphenols saw reductions of 29.4% and 36.0% in total cholesterol and LDL, respectively, while achieving an increase in HDL levels of 40.1%. All parameters in the placebo group were essentially unchanged from baseline. In the post-statin group, there was a 25.0% reduction in total cholesterol, 27.6% decrease in LDL levels, and a 23.8% increase in HDL—with none of the side effects seen earlier with statin therapy in this group. Based on these results, the bergamot polyphenols proved to be an effective therapeutic intervention for elevated cholesterol levels as well as a safe and beneficial alternative for individuals intolerant to statin drugs.
Fitoterapia. 2011 Apr;82(3):309-16.
SourceFaculty of Pharmacy, Department of Pharmacobiological Sciences, University Magna Graecia, Catanzaro, Italy.Bergamot juice produces hypolipemic activity in rats though the mechanism remains unclear. Here we investigated on the effect of bergamot extract (BPF) in diet-induced hyperlipemia in Wistar rats and in 237 patients suffering from hyperlipemia either associated or not with hyperglycaemia. BPF, given orally for 30 days to both rats and patients, reduces total and LDL cholesterol levels (an effect accompanied by elevation of cHDL), triglyceride levels and by a significant decrease in blood glucose. Moreover, BPF inhibited HMG-CoA reductase activity and enhanced reactive vasodilation thus representing an efficient phytotherapeutic approach in combating hyperlipemic and hyperglycaemic disorders.
http://atvb.ahajournals.org/
Arteriosclerosis, Thrombosis, and Vascular Biology. 2005;25:1475.
Atherosclerosis and Lipoproteins Genetic Determinants of Cardiovascular Disease Risk in Familial Hypercholesterolemia
Correspondence to John J.P. Kastelein, Department of Vascular Medicine, Academic Medical Center, Meibergdreef 9, P.O.Box 22700, room F4-159.2, 1100 DE Amsterdam, the Netherlands.
Angiology Volume 60 Number 1 February/March 2009 127-128 # 2009 SAGE Publications 10.1177/0003319708327788Letter to the Editor. After the Failure of ENHANCEd Cholesterol Lowering in Familial Hypercholesterolemia, SEAS of Problems with Ezetimibe by Luca Mascitelli, MD Uffe Ravnskov, MD, PhD Francesca Pezzetta, MD Ospedale di Tolmezzo Mark R. Goldstein, MD, FACPMounting evidence suggests that in familial hypercholesterolemia neither the incidence3 nor the prevalence4 of cardiovascular disease is associated with the lipid levels. This striking observation has been explained by the narrow range of LDL concentrations. 3The argument is untenable, however, because total and LDL cholesterol in some individuals with familial hypercholesterolemia may be more than twice as high as in others. A possible cause of cardiovascular disease in familial hypercholesterolemia may be inborn errors of the coagulation system.1 Whayne TF Jr. Is there a problem with ezetimibe or just ENHANCEd hype? Angiology. 2008 Sep 15 [Epub ahead of print].2. Pedone C, Carbonin P, Kastelein JJ, et al. ENHANCE
Investigators. Simvastatin with or without ezetimibe in
familial hypercholesterolemia. N Engl J Med. 2008;358:
1431-1443.3. Jansen AC, van Aalst-Cohen ES, Tanck MW, et al. The
contribution of classical risk factors to cardiovascular
disease in familial hypercholesterolaemia: data in 2400
patients. J Intern Med. 2004;256:482-490.4. de Sauvage Nolting PR, Defesche JC, Buirma RJ,
Hutten BA, Lansberg PJ, Kastelein JJ. Prevalence and
significance of cardiovascular risk factors in a large cohort
of patients with familial hypercholesterolaemia. J Intern
Med. 2003;253:161-168.5. SugrueDD, Trayner I,ThompsonGR, et al.Coronary artery
disease and haemostatic variables in heterozygous familial
hypercholesterolaemia. Br Heart J. 1985;53: 265-268.6. Jansen AC, van Aalst-Cohen ES, Tanck MW, et al,
Genetic determinants of cardiovascular disease risk in
familial hypercholesterolemia. Arterioscler Thromb Vasc
Biol. 2005;25:1475-1481.7. Rossebø AB, Pedersen TR, Boman K, et al. for the SEAS
Investigators. Intensive lipid lowering with simvastatin
and ezetimibe in aortic stenosis. N Engl J Med.
2008;359:1343-1356.8 Goldstein MR, Mascitelli L, Pezzetta F. The doubleedged
sword of statin immunomodulation. Int J Cardiol.
2008 May 15 [Epub ahead of print].9. Shepherd J, Blauw GJ, Murphy MB, et al, and the
PROSPER study group. PROspective Study of Pravastatin
in the Elderly at Risk. Pravastatin in elderly individuals
at risk of vascular disease (PROSPER): a randomised
controlled trial. Lancet. 2002;360:1623-1630.10. Bradford PG, Awad AB. Phytosterols as anticancer compounds.
Mol Nutr Food Res. 2007;51:161-170.11. Ravnskov U. Re: the association between statins and
cancer incidence in a veterans==============================
http://www.ncbi.nlm.nih.gov/
The contribution of classical risk factors to cardiovascular disease in familial hypercholesterolaemia: data in 2400 patients. Jansen AC, van Aalst-Cohen ES, Tanck MW, Trip MD, Lansberg PJ, Liem AH, van Lennep HW, Sijbrands EJ, Kastelein JJ. Department of Vascular Medicine, Academic Medical Centre, University of Amsterdam, 1105 AZ Amsterdam, the Netherlands.
OBJECTIVE: To determine the contribution of classical risk factors to the development of cardiovascular disease (CVD) in patients with heterozygous familial hypercholesterolaemia (FH).DESIGN: A retrospective, multi-centre, cohort study. Extensive data were collected by scrutinizing medical records and the use of questionnaires. Multivariate Cox regression was used to study the relationship between potential risk factors and the occurrence of CVD.SETTING AND SUBJECTS: We included 2400 FH patients from 27 Dutch lipid clinics. The diagnosis of FH was based upon the presence of a low-density lipoprotein receptor mutation or upon strict clinical criteria.MAIN OUTCOME MEASURES: Cardiovascular mortality and CVD.RESULTS: During 112.943 person-years, 782 (32.6%) patients had had at least one cardiovascular event. Male gender (RR 2.82, 95% CI 2.37-3.36), smoking (RR 1.67, 95% CI 1.40-1.99), hypertension (RR 1.36, 95% CI 1.06-1.75), diabetes mellitus (RR 2.19, 95% CI 1.36-3.54), low HDL-C (RR 1.37, 95% CI 1.15-1.63) and elevated lipoprotein(a) levels (RR 1.50, 95% CI 1.20-1.79) proved to be independent CVD risk factors. These six risk factors explained 18.7% of the variation in the occurrence of CVD.CONCLUSIONS: Male gender, smoking, hypertension, diabetes mellitus, HDL cholesterol and lipoprotein(a) levels proved to be important risk factors for CVD in FH patients. In addition to the routine institution of statin therapy, controlling these factors needs special attention in the management of this disorder.
——————————
Clin Chem. 2005 Nov;51(11):2067-73. Epub 2005 Sep 1.
Lipoprotein(a) is an independent risk factor for cardiovascular disease in heterozygous familial hypercholesterolemia. Holmes DT, Schick BA, Humphries KH, Frohlich J. St. Paul’s Hospital Lipid Clinic and the University of British Columbia Department of Pathology and Laboratory Medicine, Vancouver, Canada.Abstract
BACKGROUND: The role of lipoprotein(a) [Lp(a)] as a predictor of cardiovascular disease (CVD) in patients with heterozygous familial hypercholesterolemia (HFH) is unclear. We sought to examine the utility of this lipoprotein as a predictor of CVD outcomes in the HFH population at our lipid clinic.METHODS: This was a retrospective analysis of clinical and laboratory data from a large multiethnic cohort of HFH patients at a single, large lipid clinic in Vancouver, Canada. Three hundred and eighty-eight patients were diagnosed with possible, probable, or definite HFH by strict clinical diagnostic criteria. Multivariate Cox regression analysis was used to study the relationship between several established CVD risk factors, Lp(a), and the age of first hard CVD event.
RESULTS: An Lp(a) concentration of 800 units/L (560 mg/L) or higher was a significant independent risk factor for CVD outcomes [hazard ratio (HR) = 2.59; 95% confidence interval (CI), 1.53-4.39; P < 0.001].
Other significant risk factors were male sex [HR = 3.19 (1.79-5.69); P < 0.001] and ratio of total to HDL-cholesterol [1.18 (1.07-1.30); P = 0.001]. A previous history of smoking or hypertension each produced HRs consistent with increased CVD risk [HR = 1.55 (0.92-2.61) and 1.57 (0.90-2.74), respectively], but neither reached statistical significance (both P = 0.10).
LDL-cholesterol was not an independent predictor of CVD risk [HR = 0.85 (0.0.71-1.01); P = 0.07], nor was survival affected by the subcategory of HFH diagnosis (i.e., possible vs probable vs definite HFH).
CONCLUSION: Lp(a) is an independent predictor of CVD risk in a multiethnic HFH population.
——————–
http://www.ncbi.nlm.nih.gov/
Heart. 2004 Dec;90(12):1431-7.
Established and emerging coronary risk factors in patients with heterozygous familial hypercholesterolaemia. Neil HA, Seagroatt V, Betteridge DJ, Cooper MP, Durrington PN, Miller JP, Seed M, Naoumova RP, Thompson GR, Huxley R, Humphries SE. Division of Public Health & Primary Health Care, Institute of Health Sciences, University of Oxford, Old Road, Headington, Oxford OX3 7LF, UK.
Abstract
OBJECTIVES: To assess the clinical and biochemical factors associated with inter-individual variation in susceptibility to coronary artery disease (CAD) in treated heterozygous familial hypercholesterolaemia.
DESIGN: A cross sectional study was conducted of 410 patients recruited from six lipid clinics in the UK.
RESULTS: CAD was documented in 104 of the 211 men and in 55 of the 199 women with mean ages of onset of 43.1 and 46.5 years, respectively. CAD was significantly more common in men (49% v 28%, p < 0.001) and in patients who had smoked cigarettes versus patients who had never smoked (51% v 28%, p < 0.001). After adjusting for age, sex, and current smoking status, there were no significant differences between patients with or without CAD in lipoprotein(a), homocysteine, fibrinogen, plasminogen activator inhibitor-1, white blood cell count, body mass index, glucose, triglyceride or total cholesterol. However, high density lipoprotein (HDL) cholesterol concentrations were significantly lower in those with CAD (6%, 95% confidence interval (CI) 1% to 11%, p = 0.03) and this difference was greater in women than men (12% v 2%, p = 0.041).
CONCLUSIONS: These results indicate that emerging coronary risk factors appear not to be associated with CAD in adults with treated familial hypercholesterolaemia, but the strong association with smoking suggests that patients should be identified early in childhood and discouraged from ever starting to smoke.
———————-
http://www.ncbi.nlm.nih.gov/
J Med Genet. 2006 December; 43(12): 943–949.
Genetic causes of familial hypercholesterolaemia in patients in the UK: relation to plasma lipid levels and coronary heart disease risk. S E Humphries, R A Whittall, C S Hubbart, S Maplebeck, J A Cooper, A K Soutar, R Naoumova, G R Thompson, M Seed, P N Durrington, J P Miller, D J B Betteridge, and H A W Neil, for the Simon Broome Familial Hyperlipidaemia Register Group and Scientific Steering Committee S E Humphries, R A Whittall, C S Hubbart, S Maplebeck, J A Cooper, Centre for Cardiovascular Genetics, British Heart Foundation Laboratories, Royal Free and University College London Medical School, London, UKA K Soutar, R Naoumova, G R Thompson, Medical Research Council Clinical Sciences Centre, Imperial College Faculty of Medicine, Hammersmith Hospital, London, UK
——————————
http://www.atherosclerosis-
Atherosclerosis Volume 179, Issue 2 , Pages 293-297, April 2005
Non-coronary heart disease mortality and risk of fatal cancer in patients with treated heterozygous familial hypercholesterolaemia: a prospective registry study
H.A.W. Neil et al.
The prognosis from coronary heart disease (CHD) for patients with heterozygous familial hypercholesterolaemia has improved substantially since the introduction of HMG Co-A reductase inhibitors (statins), but the effect of lipid-lowering drug therapy combined with dietary and life style advice on non-coronary mortality and the risk of fatal cancer is unclear.
Methods:The cohort of 2871 patients was recruited from 21 outpatient lipid clinics in the UK from 1980 to 1998 and was followed for 22,992 person-years. The standardised mortality ratio (SMR) was calculated from the ratio of the number of deaths observed to the number expected in the general population of England and Wales.
Results:There were 169 deaths, including 102 (60.4%) from CHD, and 32 (18.9%) from cancer. The SMR for CHD was 2.5-fold higher than in the general population (95% CI 2.1, 3.1), but the all-cause SMR was not increased (1.1, 95% CI 0.9, 1.3) and non-coronary mortality was significantly lower in men (0.5, 95% CI 0.3, 0.7) and women (0.6, 95% CI 0.4, 0.9). The SMR for all cancers was significantly reduced (0.6, 95% CI 0.4, 0.8) with an 80% reduction in fatal cancers of the respiratory and intra-thoracic organs and a non-significant reduction in fatal cancers of the genitourinary and digestive organs.
Conclusions:Although the study cannot exclude the possibility that statins have anti-cancer activity, the results strongly suggest that giving advice to consume a healthy diet, increase physical activity and stop smoking is associated with a substantial reduction in mortality from cancer.
——————————
http://www.ncbi.nlm.nih.gov/
BMJ. 2001 April 28; 322(7293): 1019–1023.
Mortality over two centuries in large pedigree with familial hypercholesterolaemia: family tree mortality study.Sijbrands EJ, Westendorp RG, Defesche JC, de Meier PH, Smelt AH, Kastelein JJ. Department of Vascular Medicine and General Internal Medicine, Academic Medical Centre, Meibergdreef 9, 1105 AZ Amsterdam, Netherlands.
To estimate all cause mortality from untreated familial hypercholesterolaemia free from selection for coronary artery disease.
Design Family tree mortality study.Setting Large pedigree in Netherlands traced back to a single pair of ancestors in the 19th century.Subjects All members of pedigree aged over 20 years with 0.5 probability of carrying a mutation for familial hypercholesterolaemia.Main outcome measure All cause mortality.
Results A total of 70 deaths took place among 250 people analysed for 6950 person years. Mortality was not increased in carriers of the mutation during the 19th and early 20th century; it rose after 1915, reached its maximum between 1935 and 1964 (standardised mortality ratio 1.78, 95% confidence interval 1.13 to 2.76; P=0.003), and fell thereafter. Mortality differed significantly between two branches of the pedigree (relative risk 3.26, 95% confidence interval 1.74 to 6.11; P=0.001).
Conclusions Risk of death varies significantly among patients with familial hypercholesterolaemia. This large variability over time and between branches of the pedigree points to a strong interaction with environmental factors. Future research is required to identify patients with familial hypercholesterolaemia who are at extreme risk and need early and vigorous preventive measures.
——————————
http://www.ncbi.nlm.nih.gov/
http://www.ncbi.nlm.nih.gov/
BMJ. 2008 Nov 11;337:a2423.
Efficacy of statins in familial hypercholesterolaemia: a long term cohort study.
Versmissen J, Oosterveer DM, Yazdanpanah M, Defesche JC, Basart DC, Liem AH, Heeringa J, Witteman JC, Lansberg PJ, Kastelein JJ, Sijbrands EJ.
SourceDepartment of Internal Medicine, Erasmus University Medical Centre, PO box 2040, 3000 CA Rotterdam, Netherlands.
Abstract
OBJECTIVE: To determine the efficacy of statin treatment on risk of coronary heart disease in patients with familial hypercholesterolaemia.
DESIGN: Cohort study with a mean follow-up of 8.5 years.
SETTING: 27 outpatient lipid clinics.
SUBJECTS: 2146 patients with familial hypercholesterolaemia without prevalent coronary heart disease before 1 January 1990.
MAIN OUTCOME MEASURES: Risk of coronary heart disease in treated and “untreated” (delay in starting statin treatment) patients compared with a Cox regression model in which statin use was a time dependent variable.
RESULTS: In January 1990, 413 (21%) of the patients had started statin treatment, and during follow-up another 1294 patients (66%) started after a mean delay of 4.3 years. Most patients received simvastatin (n=1167, 33 mg daily) or atorvastatin (n=211, 49 mg daily). We observed an overall risk reduction of 76% (hazard ratio 0.24 (95% confidence interval 0.18 to 0.30), P<0.001). In fact, the risk of myocardial infarction in these statin treated patients was not significantly greater than that in an age-matched sample from the general population (hazard ration 1.44 (0.80 to 2.60), P=0.23).
CONCLUSION: Lower statin doses than those currently advised reduced the risk of coronary heart disease to a greater extent than anticipated in patients with familial hypercholesterolaemia. With statin treatment, such patients no longer have a risk of myocardial infarction significantly different from that of the general population.
We finally compared the risk of myocardial infarction in patients with familial hypercholesterolaemia who were older than 55 years (n=261, 64 men) with that in 1975 people in a subgroup of the participants in the Rotterdam study. The mean age in both subgroups was 61.6 years and both had 24.5% men as a result of stratified selection from the Rotterdam study. The absolute risk of myocardial infarction was 6.7/1000 person years in our statin treated patients, 60.5/1000 person years in our untreated patients, and 4.1/1000 person years in the sample from the Rotterdam study. Event-free survival of our statin treated patients was not significantly different from that of the Rotterdam study sample (log rank test P=0.07), whereas our untreated patients clearly had a higher risk of coronary heart disease (log rank test P<0.001) (fig 44).). After adjustment for year of birth and sex, the point estimate of risk of myocardial infarction in our treated patients with familial hypercholesterolaemia was higher than the risk in the subgroup of the Rotterdam study, but this was not significant (hazard ratio 1.44 (0.80 to 2.60), P=0.23), whereas the risk in our untreated patients was 8.7 times higher (hazard ratio 8.69 (4.77 to 15.82), P<0.001).
We report here that relatively modest doses of statins reduced the risk of coronary heart disease by about 80% in patients with familial hypercholesterolaemia. This is a much more pronounced reduction than was anticipated based on secular trends in earlier studies.7 8 We also observed that statin treated patients older than 55 years had a risk of myocardial infarction approaching that of the general population. Finally, men and women experienced similar risk reductions in our study.
http://www.ncbi.nlm.nih.gov/
———————-
http://www.
Familial Hypercholesterolemia: Why every endocrinologist should know about PCSK9 B Y PHI L I P W. CONNE L LY, PHD
Familial hypercholesterolemia
———————————–
http://www.ncbi.nlm.nih.gov/
Cholesterol Freatment Trialists’ (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005;366:1267-1278.
Lancet. 2005 Oct 8;366(9493):1267-78. .
Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins.
Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, Kirby A, Sourjina T, Peto R, Collins R, Simes R; Cholesterol Treatment Trialists’ (CTT) Collaborators.
Results of previous randomised trials have shown that interventions that lower LDL cholesterol concentrations can significantly reduce the incidence of coronary heart disease (CHD) and other major vascular events in a wide range of individuals. But each separate trial has limited power to assess particular outcomes or particular categories of participant.
METHODS:A prospective meta-analysis of data from 90,056 individuals in 14 randomised trials of statins was done. Weighted estimates were obtained of effects on different clinical outcomes per 1.0 mmol/L reduction in LDL cholesterol.
FINDINGS:During a mean of 5 years, there were 8186 deaths, 14,348 individuals had major vascular events, and 5103 developed cancer. Mean LDL cholesterol differences at 1 year ranged from 0.35 mmol/L to 1.77 mmol/L (mean 1.09) in these trials. There was a 12% proportional reduction in all-cause mortality per mmol/L reduction in LDL cholesterol (rate ratio [RR] 0.88, 95% CI 0.84-0.91; p<0.0001). This reflected a 19% reduction in coronary mortality (0.81, 0.76-0.85; p<0.0001), and non-significant reductions in non-coronary vascular mortality (0.93, 0.83-1.03; p=0.2) and non-vascular mortality (0.95, 0.90-1.01; p=0.1). There were corresponding reductions in myocardial infarction or coronary death (0.77, 0.74-0.80; p<0.0001), in the need for coronary revascularisation (0.76, 0.73-0.80; p<0.0001), in fatal or non-fatal stroke (0.83, 0.78-0.88; p<0.0001), and, combining these, of 21% in any such major vascular event (0.79, 0.77-0.81; p<0.0001). The proportional reduction in major vascular events differed significantly (p<0.0001) according to the absolute reduction in LDL cholesterol achieved, but not otherwise. These benefits were significant within the first year, but were greater in subsequent years. Taking all years together, the overall reduction of about one fifth per mmol/L LDL cholesterol reduction translated into 48 (95% CI 39-57) fewer participants having major vascular events per 1000 among those with pre-existing CHD at baseline, compared with 25 (19-31) per 1000 among participants with no such history. There was no evidence that statins increased the incidence of cancer overall (1.00, 0.95-1.06; p=0.9) or at any particular site.
INTERPRETATION: Statin therapy can safely reduce the 5-year incidence of major coronary events, coronary revascularisation, and stroke by about one fifth per mmol/L reduction in LDL cholesterol, largely irrespective of the initial lipid profile or other presenting characteristics. The absolute benefit relates chiefly to an individual’s absolute risk of such events and to the absolute reduction in LDL cholesterol achieved. These findings reinforce the need to consider prolonged statin treatment with substantial LDL cholesterol reductions in all patients at high risk of any type of major vascular event.
Mohrschladt 2004
http://www.ncbi.nlm.nih.gov/
Atherosclerosis. 2004 Feb;172(2):329-35.
Cardiovascular disease and mortality in statin-treated patients with familial hypercholesterolemia. Mohrschladt MF, Westendorp RG, Gevers Leuven JA, Smelt AH.
Source Department of General Internal Medicine, Leiden University Medical Center, P.O. Box 9600, 2300 RC Leiden, The Netherlands.
Patients with familial hypercholesterolemia (FH) are at an increased risk of premature cardiovascular disease (CVD). The benefits of statin therapy are not well known since no placebo controlled studies have been performed in these patients. The aim of this study was to determine the CVD event and mortality risk in statin-treated patients with FH. A total of 345 FH patients were followed prospectively for 8 years. Mortality from CVD was compared to that of the general population. The absolute risk of CVD in patients without a previous history of CVD was 3% per year for men and 1.6% for women. Mortality from CVD in patients without a previous history was 1.4-fold (95% CI = 0.6-3.3) increased and ischaemic heart disease (IHD) mortality was 2.6-fold (95% CI = 1.1-6.3) higher compared to the general population.
Heart. 2011 Jul;97(14):1151-7. doi: 10.1136/hrt.2010.220699. Epub 2011 May 12.
CT coronary plaque burden in asymptomatic patients with familial hypercholesterolaemia.
Neefjes LA, Ten Kate GJ, Rossi A, Galema-Boers AJ, Langendonk JG, Weustink AC, Moelker A, Nieman K, Mollet NR, Krestin GP, Sijbrands EJ, de Feyter PJ.
SourceDepartment of Radiology and Cardiology, Erasmus Medical Center Rotterdam, CA, Rotterdam, The Netherlands.OBJECTIVE:To determine the calcium score and coronary plaque burden in asymptomatic statin-treated patients with heterozygous familial hypercholesterolaemia (FH) compared with a control group of patients with low probability of coronary artery disease, having non-anginal chest pain, using CT.
DESIGN, SETTING AND PATIENTS:101 asymptomatic patients with FH (mean age 53 ± 7 years; 62 men) and 126 patients with non-anginal chest pain (mean age 56 ± 7 years; 80 men) underwent CT calcium scoring and CT coronary angiography. All patients with FH were treated with statins during a period of 10 ± 8 years before CT. The coronary calcium score and plaque burden were determined and compared between the two patient groups.
RESULTS:The median total calcium score was significantly higher in patients with FH (Agatston score = 87, IQR 5-367) than in patients with non-anginal chest pain (Agatston score = 7, IQR 0-125; p < 0.001). The overall coronary plaque burden was significantly higher in patients with FH (p < 0.01). Male patients with FH, whose low-density lipoprotein cholesterol levels were reduced by statins below 3.0 mmol/l, had significantly less coronary calcium (p < 0.01) and plaque burden (p = 0.02).
CONCLUSION:The coronary plaque burden is high in asymptomatic middle-aged patients with FH despite intense statin treatment.http://www.ncbi.nlm.nih.gov/
Atherosclerosis. 2012 Jun;222(2):468-72. doi: 10.1016/j.atherosclerosis.
Detection of subclinical atherosclerosis in familial hypercholesterolemia using non-invasive imaging modalities.
Caballero P, Alonso R, Rosado P, Mata N, Fernández-Friera L, Jiménez-Borreguero LJ, Badimon L, Mata P.
Source Department of Radiology, Hospital de la Princesa, Madrid, Spain.To investigate the extent of subclinical atherosclerosis in asymptomatic familial hypercholesterolemia (FH) patients using non-invasive images techniques.
PATIENTS, METHODS AND RESULTS:The atherosclerotic burden of 36 molecularly defined FH patients (18 males, 45.7±10.9 years) without evidence of cardiovascular disease receiving lipid-lowering treatment and 19 (47.8±11.3 years) controls was investigated. Descending thoracic aorta magnetic resonance imaging (MRI) was performed in a 1.5 T equipment with T1 and T2 sequences to characterize atherosclerotic plaques and to measure aortic wall volumen. Carotid intima-media thickness (cIMT) and presence of plaques were measured using B-mode carotid ultrasound. Mean aortic wall volumen, cIMT and atherosclerotic plaques in aorta were significantly higher in FH cases (P<0.001). A significant correlation between aortic wall volume and cIMT was observed (P<0.01). Aortic MRI detected plaques in 94% and carotid ultrasound in 14% of cases. Lipid-rich plaques were observed only in FH cases (33%) and were associated with family history of premature coronary artery disease (P<0.05).
CONCLUSIONS:Asymptomatic middle-aged FH patients have significantly higher atherosclerotic burden than controls. cIMT has shown a significant correlation with aortic wall volume and MRI allowed the detection of lipid-rich plaques in FH subjects that were associated with family history of premature coronary artery disease.http://www.ncbi.nlm.nih.gov/
Atherosclerosis. 2011 Dec;219(2):721-7. doi: 10.1016/j.atherosclerosis.
Accelerated subclinical coronary atherosclerosis in patients with familial hypercholesterolemia.
Neefjes LA, Ten Kate GJ, Alexia R, Nieman K, Galema-Boers AJ, Langendonk JG, Weustink AC, Mollet NR, Sijbrands EJ, Krestin GP, de Feyter PJ.
Source Department of Radiology, Erasmus Medical Center, Rotterdam, The Netherlands.We determined the extent, severity, distribution and type of coronary plaques in cardiac asymptomatic patients with familial hypercholesterolemia (FH) using computed tomography (CT).
BACKGROUND:FH patients have accelerated progression of coronary artery disease (CAD) with earlier major adverse cardiac events. Non-invasive CT coronary angiography (CTCA) allows assessing the coronary plaque burden in asymptomatic patients with FH.
MATERIALS AND METHODS:A total of 140 asymptomatic statin treated FH patients (90 men; mean age 52 ± 8 years) underwent CT calcium scoring (Agatston) and CTCA using a Dual Source CT scanner with a clinical follow-up of 29 ± 8 months. The extent, severity (obstructive or non-obstructive plaque based on >50% or <50% lumen diameter reduction), distribution and type (calcified, non-calcified, or mixed) of coronary plaque were evaluated.
RESULTS:The calcium score was 0 in 28 (21%) of the patients. In 16% of the patients there was no CT-evidence of any CAD while 24% had obstructive disease. In total 775 plaques were detected with CT coronary angiography, of which 11% were obstructive. Fifty four percent of all plaques were calcified, 25% non-calcified and 21% mixed. The CAD extent was related to gender, treated HDL-cholesterol and treated LDL-cholesterol levels. There was a low incidence of cardiac events and no cardiac death occurred during follow-up.
CONCLUSION:Development of CAD is accelerated in intensively treated male and female FH patients. The extent of CAD is related to gender and cholesterol levels and ranges from absence of plaque in one out of 6 patients to extensive CAD with plaque causing >50% lumen obstruction in almost a quarter of patients with FH.http://www.ncbi.nlm.nih.gov/
Atherosclerosis. 2010 Dec;213(2):486-91. doi: 10.1016/j.atherosclerosis.
Evaluation of subclinical atherosclerosis by computed tomography coronary angiography and its association with risk factors in familial hypercholesterolemia.
Miname MH, Ribeiro MS 2nd, Parga Filho J, Avila LF, Bortolotto LA, Martinez LR, Rochitte CE, Santos RD.
Source Lipid Clinic Heart Institute (InCor), University of São Paulo, Medical School Hospital, São Paulo, Brazil.Increasing age and cholesterol levels, male gender, and family history of early coronary heart disease (CHD) are associated with early onset of CHD in familial hypercholesterolemia (FH).
OBJECTIVE:Assess subclinical atherosclerosis by computed tomography coronary angiography (CTCA) and its association with clinical and laboratorial parameters in asymptomatic FH subjects.
METHODS:102 FH subjects (36% male, 45 ± 13 years, LDL-c 280 ± 54 mg/dL) and 35 controls (40% male, 46 ± 12 years, LDL-c 103 ± 18 mg/dL) were submitted to CTCA. Plaques were divided into calcified, mixed and non-calcified; luminal stenosis was characterized as >50% obstruction.
RESULTS:FH had a greater atherosclerotic burden represented by higher number of patients with: plaques (48% vs. 14%, p=0.0005), stenosis (19% vs. 3%, p=0.015), segments with plaques (2.05 ± 2.85 vs.0.43 ± 1.33, p=0.0016) and calcium scores (55 ± 129 vs. 38 ± 140, p=0.0028). After multivariate analysis, determinants of plaque presence were increasing age (OR=2.06, for age change of 10 years, CI95%: 1.38-3.07, p<0.001) and total cholesterol (OR=1.86, for cholesterol change by 1 standard deviation, CI95%: 1.09-3.15, p=0.027). Coronary calcium score was associated with the presence of stenosis (OR=1.54; CI95%: 1.27-1.86, p<0.001, for doubling the calcium score). Male gender was directly associated with the presence of non-calcified plaques (OR: 15.45, CI95% 1.72-138.23, p=0.014) and inversely with calcified plaques (OR=0.21, CI95%: 0.05-0.84, p=0.027). Family history of early CHD was associated with the presence of mixed plaques (OR=4.90, CI95%: 1.32-18.21, p=0.018).
CONCLUSIONS:Patients with FH had an increased burden of coronary atherosclerosis by CTCA. The burden of atherosclerosis and individual plaque subtypes differed with the presence of other associated risk factors, with age and cholesterol being most important. A coronary calcium score of zero ruled out obstructive disease in this higher risk population.http://www.ncbi.nlm.nih.gov/
Am J Cardiol. 2013 Apr 1;111(7):955-61.
Coronary computed tomographic angiographic findings in asymptomatic patients with heterozygous familial hypercholesterolemia and null allele low-density lipoprotein receptor mutations.
Viladés Medel D, Leta Petracca R, Carreras Costa F, Cardona Olle M, Barros Membrilla A, Hidalgo Perez JA, Pujadas Olano S, Alomar Serrallach X, Franco Peral M, Pons-Lladó G.
Source Cardiac Imaging Unit, Cardiology Department, Universitat Autònoma de Barcelona, Barcelona, Spain.Heterozygous familial hypercholesterolemia (HeFH) can be associated with early coronary artery disease (CAD) in asymptomatic patients. The objectives of the present study were to assess the prevalence and magnitude of subclinical CAD in patients with HeFH using coronary computed tomographic angiography (CCTA) and to determine the clinical and genetic profile of those at the greatest risk of CAD. The study included 50 consecutive patients with HeFH diagnosed according to the Dutch Lipid Clinic Network criteria and a control group of 70 healthy subjects. The findings from CCTA for the patients with HeFH were compared with those from the control group, who had been referred for CCTA as a part of a preventive medical examination. In 82% of the patients with HeFH, genetic DNA was screened for low-density lipoprotein receptor (LDLR) gene mutations using a microarray. CCTA revealed a significantly greater Agatston calcium score in the study group than in the control group (260 vs 46; p = 0.002). The prevalence of CAD in the patients with HeFH was 48%. It was significant in 26%, involving mainly the proximal segments of the coronary arteries. In the control group, the prevalence of CAD was 33% and was significant in 5% (p <0.05 for prevalence and severity of CAD compared to patients with HeFH). In those with HeFH, increased age, null allele LDLR mutations, and low high-density lipoprotein blood levels at diagnosis showed a statistically significant association with CAD (p <0.05). In conclusion, patients with HeFH present with a greater prevalence, extension, and severity of subclinical CAD than the general population. Increased age, low high-density lipoprotein levels, and LDLR null allele mutations are related to the occurrence of CAD. CCTA has emerged as a useful technique for the screening of subclinical CAD in patients with HeFH.——————————–
From: Jeffrey Dach <drdach@drdach.com>
Date: Fri, Jul 5, 2013 at 4:38 PM
Subject: Bergamot
To: Jeffrey Dach MD TrueMedMD <jdach@bellsouth.net>
Cc: Jeffrey Dach MD TrueMedMD <drdach@drdach.com>http://www.ncbi.nlm.nih.gov/
JAMA. 1986 Jan 10;255(2):219-24.
Evidence that men with familial hypercholesterolemia can avoid early coronary death. An analysis of 77 gene carriers in four Utah pedigrees.
Williams RR, Hasstedt SJ, Wilson DE, Ash KO, Yanowitz FF, Reiber GE, Kuida H.
AbstractTo study the genetic influence on serum cholesterol levels and early coronary heart disease, 1,134 individuals were screened from 18 Utah pedigrees. In most pedigrees, serum cholesterol appeared to be a purely polygenic trait, with 54% heritability. In four pedigrees with dominant familial hypercholesterolemia, male heterozygotes had a mean serum cholesterol level of 352 mg/dL, myocardial infarction at an average age of 42 years, and coronary death at an average age of 45 years. An informative pedigree structure allowed the identification of four ancestral males born before 1880 who carried this lethal gene and survived to ages 62, 68, 72, and 81 years. This suggests that some healthy life-style factors protected these men against the expression of a gene that has led to coronary disease by age 45 years in all of their heterozygous great-grandsons. One heterozygote showed a drop in serum cholesterol level from 426 to 248 mg/dL, with strict adherence to a low-fat diet without drugs. These observations should help encourage physicians to try harder to identify and help such individuals.http://circ.ahajournals.org/
http://www.ncbi.nlm.nih.gov/
Circulation. 1995 Aug 1;92(3):290-5.
Coronary artery disease in heterozygous familial hypercholesterolemia patients with the same LDL receptor gene mutation.
Ferrières J, Lambert J, Lussier-Cacan S, Davignon J.
SourceDépartement de médecine sociale et préventive, Faculté de Médecine, Université de Montréal, Quebec, Canada.
Abstract
BACKGROUND:Familial hypercholesterolemia (FH), an autosomal codominant disease, is characterized by high levels of LDL cholesterol and a high incidence of coronary artery disease (CAD). To date, genetic heterogeneity has hindered the proper assessment of the relation between risk factors and CAD in FH patients.
METHODS AND RESULTS:We studied the association between CAD and common risk factors in a sample of 263 French Canadian FH patients (147 women, 116 men) carrying the same > 10-kb deletion of the LDL receptor gene. Thirty-five women and 54 men had CAD. The mean age of onset of CAD was 45.6 +/- 12.7 years in women and 38.8 +/- 9.4 years in men. Multiple logistic regression analyses were performed to test the association between CAD and age, tendon xanthomas, cigarette smoking, hypertension, diabetes mellitus, apolipoprotein E polymorphism, total plasma cholesterol, triglycerides, VLDL cholesterol, LDL cholesterol, HDL cholesterol, and lipoprotein(a) [Lp(a)]. In FH women, significant multivariate predictors were age (odds ratio, 1.10 for 1 year; P < .0001), VLDL cholesterol (odds ratio, 3.85 for 1 natural log unit; P < .002), and LDL cholesterol (odds ratio, 1.42 for 1 mmol/L; P < .02). In FH men, age (odds ratio, 1.08 for 1 year; P < .0001) and HDL cholesterol (odds ratio, 0.14 for 1 mmol/L; P = .05) were significant predictors of disease. Lp(a) was not a significant predictor in univariate or multivariate analyses.
CONCLUSIONS:This study suggests that increased risk of CAD in FH is not solely due to elevated LDL cholesterol levels and demonstrates a sex-specific lipoprotein influence on CAD in a large sample of FH patients carrying the same LDL receptor gene defect.http://atvb.ahajournals.org/
http://www.ncbi.nlm.nih.gov/
Arterioscler Thromb Vasc Biol. 2005 Jul;25(7):1475-81. Epub 2005 May 5.
Genetic determinants of cardiovascular disease risk in familial hypercholesterolemia.
Jansen AC, van Aalst-Cohen ES, Tanck MW, Cheng S, Fontecha MR, Li J, Defesche JC, Kastelein JJ.
Source Department of Vascular Medicine, Academic Medical Center, Amsterdam, The Netherlands.
Abstract OBJECTIVE: To investigate the contribution of polymorphisms in multiple candidate genes to cardiovascular disease (CVD) risk in a large cohort of patients with heterozygous familial hypercholesterolemia (FH).
METHODS AND RESULTS: We genotyped 1940 FH patients for 65 polymorphisms in 36 candidate genes. During 91.451 person-years, 643 (33.1%) patients had at least 1 cardiovascular event. Multifactorial Cox survival analysis revealed that the G20210A polymorphism in the prothrombin gene was strongly associated with a significantly increased CVD risk (GA versus GG; P<0.001).
CONCLUSIONS: In a large cohort of FH patients, we found that the G20210A polymorphism in the prothrombin gene is strongly associated with CVD risk. Our results constitute a step forward in the unraveling of the hereditary propensity toward CVD in FH and might lead to better risk stratification and hence to more tailored therapy for CVD prevention.http://www.ncbi.nlm.nih.gov/
Br Heart J. 1985 Mar;53(3):265-8.
Coronary artery disease and haemostatic variables in heterozygous familial hypercholesterolaemia.
Sugrue DD, Trayner I, Thompson GR, Vere VJ, Dimeson J, Stirling Y, Meade TW.
Abstract Haemostatic variables were measured in 61 patients with heterozygous familial hypercholesterolaemia, 32 of whom had evidence of coronary heart disease. Age adjusted mean concentrations of plasma fibrinogen and factor VIII were significantly higher in these patients than in the 29 patients without coronary heart disease, but there were no significant differences in serum lipid concentrations between the two groups. Comparisons in 30 patients taking and not taking lipid lowering drugs showed lower values for low density lipoprotein cholesterol, high density lipoprotein cholesterol and antithrombin III, and a higher high density lipoprotein ratio while receiving treatment. The results suggest that hypercoagulability may play a role in the pathogenesis of coronary heart disease in patients with familial hypercholesterolaemia.http://www.ncbi.nlm.nih.gov/
Mortality in treated heterozygous familial hypercholesterolaemia: implications for clinical management. Scientific Steering Committee on behalf of the Simon Broome Register Group.
[No authors listed] AbstractClinical management of heterozygous familial hypercholesterolaemia is largely based on evidence from a small number of observational studies and extrapolation from the results of clinical trials of lipid-lowering in patients with polygenic hypercholesterolaemia The objectives of this study were (i) to determine the absolute and relative mortality of patients with treated heterozygous familial hypercholesterolaemia, (ii) to estimate the effect of changes in treatment efficacy on mortality trends over time, and (iii) to examine the implications of these findings for patient management. A cohort of 605 men and 580 women aged 20-79 years with heterozyous familial hypercholesterolaemia were recruited from 21 out-patient lipid clinics in the UK. Patients were followed prospectively from 1980 to 1995 for 8770 person-years. Absolute mortality was calculated, and relative risk was expressed as the ratio of the number of observed deaths to the number expected in the general population of England and Wales. Forty six of the 73 deaths were due to coronary heart disease. In women aged 20-39, despite treatment, the relative risk of a fatal coronary event was increased 125-fold (95% confidence intervals 15-451) and the annual coronary mortality was 0.17%. In men aged 20-39 the relative risk was increased 48-fold (17-105) and the annual coronary mortality was 0.46%. The relative risk decreased with age but the absolute risk increased. For men and women aged 60-79, the annual coronary mortality was 1.1% representing a significant excess mortality for women (relative risk 2.6, 1.3-4.5) but not for men (RR 1.1, 0.5-2.3). Non-coronary mortality was not increased at any age (RR for all ages 0.68, 0.45-0.99). There was a decline in the relative risk for coronary mortality in patients aged 20-59 from an eight-fold (4.8-7.2) increased risk before 1992 to 3.7 (1.6-7.2.) thereafter (P=0.08). The results suggest that the prognosis for patients with heterozygous familial hypercholesterolaemia has improved with the introduction of more effective treatment, and that lipid-lowering therapy is not associated with increased non-coronary mortality. These findings and the excess coronary mortality observed suggest that all affected adult men and post-menopausal women should be treated with HMG-CoA reductase inhibitors.
Benefits of high cholesterol
‘
http://www.ravnskov.nu/the%
http://www.ncbi.nlm.nih.gov/
Age Ageing. 2010 Nov;39(6):674-80. doi: 10.1093/ageing/afq129. Epub 2010 Oct 14.
Lipid-lowering treatment to the end? A review of observational studies and RCTs on cholesterol and mortality in 80+-year olds.
Petersen LK, Christensen K, Kragstrup J.
Source
Research Unit of Epidemiology, Danish Aging Research Center, University of Southern Denmark, Odense, Denmark. lkpetersen@health.sdu.dk
Abstract
People aged 80 or older are the fastest growing population in high-income countries. One of the most common causes of death among the elderly is the cardiovascular disease (CVD). Lipid-lowering treatment is common, e.g. one-third of 75-84-year-old Swedes are treated with statins. The assumption that hypercholesterolaemia is a risk factor at the highest ages seems to be based on extrapolation from younger adults. A review of observational studies shows a trend where all-cause mortality was highest when total cholesterol (TC) was lowest (‘a reverse J-shaped’ association between TC and all-cause mortality). Low TC (<5.5 mmol/l) is associated with the highest mortality rate in 80+-year olds. No clear optimal level of TC was identified. A review of the few randomised controlled trials including 80+-year olds did not provide evidence of an effect of lipid-lowering treatment on total mortality in 80+-year-old people. There is not sufficient data to recommend anything regarding initiation or continuation of lipid-lowering treatment for the population aged 80+, with known CVD, and it is even possible that statins may increase all-cause mortality in this group of elderly individuals without CVD.
————————-

Jeffrey Dach MD
http://www.jeffreydach.com/
http://www.drdach.com/
http://www.naturalmedicine101.com/
http://www.truemedmd.com/
Disclaimer click here: http://www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship. Although identities will remain confidential as much as possible, as I can not control the media,
I can not take responsibility for any breaches of confidentiality that may occur.
Link to this article: http://wp.me/p3gFbV-tl
Copyright (c) 2009-2013 Jeffrey Dach MD All Rights Reserved. This article may be reproduced on the internet without permission, provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.










Leave a Comment
You must be logged in to post a comment.