 Selling Sickness in the Lobby, Fast Food in Hospitals by Jeffrey Dach MD
Selling Sickness in the Lobby, Fast Food in Hospitals by Jeffrey Dach MDPeter Cram reported in JAMA that forty per cent of hospitals have fast food in the lobby. While you might consider this an outrage, its just business. Above Image Courtesy of Wikimedia, Fast food restaurant Shinjuku-i-land, Tokyo.
Your hospital banned cigarette smoking long ago, yet still give the impression that fast food is healthy for you. The reality is that fast food causes chronic disease, a lucrative source for new revenue. If you were the hospital accountant, you would consider this extra income a good thing. Financial gain, rather than the health is the over-riding consideration.
Untrained in medical nutrition, hospital accountants may not understand that fast food causes obesity, metabolic syndrome, insulin resistant diabetes, hypertension and accelerated cardiovascular disease. (1-7)
 Michael Pollen, a journalist and author of “In Defense of Food”, and “Food Rules” says in a New York Times Editorial that fast food causes chronic disease, and he says:
Michael Pollen, a journalist and author of “In Defense of Food”, and “Food Rules” says in a New York Times Editorial that fast food causes chronic disease, and he says:
“there’s lots of money to be made selling fast food, and then treating the diseases that fast food causes. One of the leading products of the American food industry has become patients for the American health care industry“. (8)
You might ask, what is the evidence that fast food causes obesity and chronic disease? For starters. a 2004 study published in Lancet found that eating at a Fast Food restaurant causes weight gain and insulin resistance. (29)(30) The authors say,
“fast foods contain large amounts of partially hydrogenated oils, and this class of fatty acids can cause insulin resistance and increase risk of type 2 diabetes. Fast food also contains large amounts of highly refined starchy food and added sugar, carbohydrates that have been characterized as high in glycemic index. Consumption of a high glycemic index or high glycaemic load diet has been linked to risk for diabetes, independent of bodyweight changes...”
Watch this video about how “unfit meat” can be used as hamburgers. Chef Jamie Oliver says the fatty parts of beef are “washed” in ammonium hydroxide and then used as hamburger. This meat is actually unfit for human consumption and is intended as dog food… “Basically, we’re taking a product that would be sold in the cheapest way for dogs, and after this process, is being given to human beings..a pink slime process.”
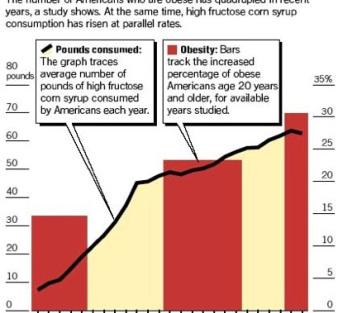
The chart below shows the national obesity epidemic rising at parallel rates with refined sugar consumption, mostly in the form of high fructose corn syrup (HFCS). The average American consumes 70 pounds a year of refined sugar.
 Health Risks of Sugar Consumption – HFCS
Health Risks of Sugar Consumption – HFCSIgnoring for the moment the hydrogenated vegetable oils in fast food which are an enormous health risk, let’s focus on the sweeteners, the high fructose corn syrup used in fast food and soft drinks. The evidence linking massive amounts of sugar consumption to chronic disease is overwhelming. (9-27)
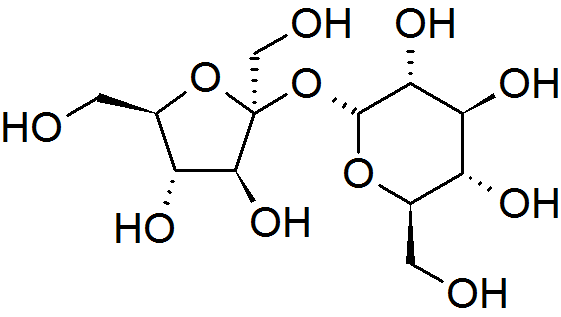 Image above: Table sugar, Sucrose molecule courtesy of wikimedia.
Image above: Table sugar, Sucrose molecule courtesy of wikimedia.
High Fructose Corn Syrup is the preferred sweetener, refined from government subsidized corn and used for processed foods. HFCS is cheaper and sweeter than regular table sugar (sucrose), and it prolongs shelf life. High Fructose corn syrup is a 4.5 BILLION dollar industry, with our annual sugar consumption at 73.5 lbs per person. Now, thats a lot of sugar!
 Left image: refined sugar crystals courtesy of wikimedia commons.
Left image: refined sugar crystals courtesy of wikimedia commons.
Some scientists say that refined table sugar (sucrose) is not food, and should be reclassified as a drug capable of producing craving, withdrawal effects and addiction. A 2002 Princeton study showed addictive behaviors in rats given intermittent high sugar intake. A 2008 report in NeuroScience examines the evidence for addiction associated with intermittent excess sugar intake.
The scientific evidence of sugar addiction is summarized nicely by Kathleen DesMaisons, Ph.D., author of The Sugar Addict’s Total Recovery Program, and Potatoes Not Prozac. Her program, called RadiantRecovery, is dedicated to helping people overcome sugar addition.
 Chemically speaking, HFCS is a mixture of 55% fructose and 45% glucose, a ratio intended to mimic common table sugar, called sucrose. Sucrose is a simple molecule made of one fructose and one glucose molecule, so the corn industry can say that
Chemically speaking, HFCS is a mixture of 55% fructose and 45% glucose, a ratio intended to mimic common table sugar, called sucrose. Sucrose is a simple molecule made of one fructose and one glucose molecule, so the corn industry can say that
sucrose and HFCS are the same stuff. Of course this is partially true, but there is a difference. Firstly, HFCS has 10% more fructose than table sugar. Secondly the fructose in HFCS is  absorbed into the bloodstream more rapidly, since the body must first cleave apart sucrose with enzymatic digestion, after which, the liberated fructose can be absorbed into the bloodstream. Once absorbed, fructose and glucose are metabolized quite differently.
absorbed into the bloodstream more rapidly, since the body must first cleave apart sucrose with enzymatic digestion, after which, the liberated fructose can be absorbed into the bloodstream. Once absorbed, fructose and glucose are metabolized quite differently.
Intravenous glucose is commonly given to patients in the hospital to sustain life. There is no IV fructose in the bag, however. Why is this? Because IV fructose is dangerous.
 Left Image : Bag of Intravenous Glucose (also called dextrose) Courtesy of WIkimedia Commons.
Left Image : Bag of Intravenous Glucose (also called dextrose) Courtesy of WIkimedia Commons.
Health Risks of Fructose in Fast Food Sodas
In small amounts, fructose has always been a healthy part of human diet in fruits and vegetables. However, large amounts of fructose poses a serious health risk. Unlike glucose, fructose cannot be used by the body. Instead, it must be processed in the liver where it is uncontrollably converted into fat particles, triglycerides and atherogenic lipids. This causes insulin resistant diabetes, hypertension and cardiovascular disease. Thus, fructose is considered more dangerous and harmful than plain old glucose. Fructose also causes abnormal lipid panels in obese kids, who may then be given statin drugs. Wouldn’t it make more sense to cut out the fructose instead?(9-27)
 A recent CDC report raises alarms about increasing teen obesity and high cholesterol found in 20% of kids. The CDC report went on to recommend that doctors adhere to guidelines calling for statin drugs for kids with high cholesterol.
A recent CDC report raises alarms about increasing teen obesity and high cholesterol found in 20% of kids. The CDC report went on to recommend that doctors adhere to guidelines calling for statin drugs for kids with high cholesterol.
In 1998, the American Academy of Pediatrics convened a Committee on Nutrition to discuss “Cholesterol in Childhood ” which published guidelines for treating kids with statin drugs for high cholesterol. The guidlines were revised in 2008 by Dr Stephen R. Daniels, causing a national uproar. Apparently, Daniels and co-authors had undisclosed ties to Merck, maker of statin drug Mevacor.
The problem with cholesterol guidelines for kids is absence of any medical data showing benefit from statin drugs in this age group. Alternatively, we have plenty of evidence that statin drugs cause harmful adverse side effects, especially considering a child starting statins is committed to 40 years of drug treatment. Articles promptly appeared in the media and medical literature (Storm over Statins) raising opposition and creating backlash against the guidelines for statin drugs for kids. In view of what we know about Fast Food causing teen obesity and abnormal lipid panels, it would seem the height of absurdity to give kids statin drugs, rather than address the fast food and soda pop diets.
 Another problem with fast food in the lobby, is fecal contamination of soda fountains, reported in the Jan 2010 issue of the International Journal of Food Microbiology.
Another problem with fast food in the lobby, is fecal contamination of soda fountains, reported in the Jan 2010 issue of the International Journal of Food Microbiology.
Take Action ! Make a copy this article and give it to your local congressman, or hospital board member.
Update:
Mayor Michael Bloomberg is aiming to banish sugary and fatty foods from both public and private hospitals.
Countering Fast Food’s Health Effects
NHS hospitals fueling obesity crisis with fast food outlets
Articles with Related Interest
Grocery Store as Minefield Avoiding the Dangers
Links and References
FAST FOODS IN HOSPITAL LOBBY
(1) http://pediatrics.aappublications.org/cgi/content/full/118/6/2290?vm=t
PEDIATRICS Vol. 118 No. 6 December 2006 Marketing Fast Food: Impact of Fast Food Restaurants in Children’s Hospitals, Hannah B. Sahud, MD et al.
Department of Pediatrics, Children’s Memorial Hospital, Northwestern University
Fifty-nine of 200 hospitals with pediatric residencies had fast food restaurants. We found that fast food restaurants were reported in 29.5% of hospitals that sponsor pediatric residency programs, a figure that is similar to that reported previously in general hospitals.14 We also present the first documentation that the presence of a McDonald’s restaurant in a children’s hospital was associated with (1) increased fast food purchasing by parents, (2) the belief that McDonald’s Corporation was a hospital benefactor, and (3) more positive perceptions of the healthiness of McDonald’s food.
However, the presence of fast food restaurants in pediatric hospitals markets dietary choices that are contrary to desired health messages.29
Fast food restaurants are found in 29.5% of US hospitals with pediatric residency programs. The presence of a McDonald’s restaurant in a children’s hospital significantly increased the purchase of fast food on the day of a hospital outpatient visit, mostly as a result of purchase of food at the in-hospital McDonald’s. Moreover, the presence of an on-site McDonald’s restaurant was significantly associated with a more positive perception of McDonald’s food and with the belief that McDonald’s Corporation is a financial supporter of the hospital.
the presence of fast food franchises in hospitals contributes to parental perceptions of fast food quality at a time when childhood obesity is increasing. In the midst of increasing rates of childhood obesity, efforts are needed to balance the dietary choices and social messages consequent to the presence of fast food restaurants in children’s hospitals. The presence of fast food restaurants in children’s hospitals should be reconsidered.
(2) http://www.jabfm.org/cgi/content/full/19/5/526
Prevalence and Type of Brand Name Fast Food at Academic-affiliated Hospitals The Journal of the American Board of Family Medicine 19:526-527 (2006) Lenard I. Lesser, MD Tufts University Family Medicine Residency, Malden, MA
Conclusions Among the 234 academic-affiliated hospitals surveyed, 42% had BNFF served on their campus. This percentage is similar to that reported by Cram et al,10 who found that 38% of the top 16 hospitals in the United States had fast food establishments. McDonald et al11 reported that 9% of children’s hospitals (including academic and non-academic) in North America had BNFF franchises. However, in the present study we included food served in restaurants and also brand name products available in other venues on campus.
Others have studied the location of BNFF franchises. One study showed a positive association between the state level of obesity and the number of Burger Kings and McDonalds per person or per square mile.12 Moreover, although 35% of Chicago schools had a fast food franchise within 400 meters,9 this study confirms that they are also prevalent in close proximity to (ie, on the grounds of) many hospitals/medical centers.
Our study also reports the most common types of BNFF in hospitals. As nutritional information on BNFF is available on most company Web sites, the readership can use this data to make its own judgments on the nutritional quality of some of the food offered by academic-affiliated hospitals. Some hospital administrators have attempted, with some success, to remove what they deemed as unhealthy fast food from their premises. For instance, at the Cleveland Clinic, the Pizza Hut was removed from the hospital, but McDonalds remained.13 Administrators at teaching hospitals should continue to consider whether the food they serve on their campuses is consistent with the mission of improving the health of their communities. Future studies should continue to characterize the types of food available in all venues on medical center campuses.
Frequency of Brand Name Fast Food (BNFF) Franchises at 233 Academically Affiliated Hospitals Brand Name Fast Food Franchise Number of Hospital Campuses Hosting a BNFF
Krispy Kreme 23
Subway 21
Burger King, McDonalds 16 of each
Au Bon Pain, Pizza Hut 10 of each
ChickfilA 7
Wendy’s 6
Chipotle, Dunkin Donuts, Einstein’s Bagels, KFC, Quizno’s, Starbucks 4 of each
Taco Bell 3
Sbarro, TCBY, Freshen’s Yogurt 2 of each
Amante’s Pizza, Blimpie, Carvel, Chicken Kitchen, Dairy Queen, Dangelo’s, Dominos, El Pollo Loco, Gloria Jean Coffee, Goldstar Chili, Hardees, Hovan, LaRosa’s Pizza, Little Dino’s, Miami Subs, Mr.Goodcent’s, Mrs.Fields, Panda Express, Papa John’s, Pizza Inn, Tim Hortons
(3) http://jama.ama-assn.org/cgi/content/full/287/22/2945
Vol. 287 No. 22, June 12, 2002 JAMA by Peter Cram, MD
Fast Food Franchises in Hospitals
The incidence of obesity is rising at an alarming rate in the United States, with nearly 18% of adult Americans now considered obese.1 High-calorie diets, due in part to the proliferation of fast food restaurants, are an important contributing factor.2 Surprisingly, hospitals—institutions traditionally involved in the promotion of health-related behavior—are increasingly contracting with fast food franchises that frequently offer limited, high-fat, high-calorie menus.3 The prevalence of such franchises in hospitals across the United States is not known.
Methods – We performed a telephone survey of 16 facilities listed as “Honor Roll” hospitals by the 2001 US News & World Report on “America’s Best Hospitals.”4
Results – All 16 hospitals responded to the survey. Six of the 16 (38%) hospitals had regional or national fast food franchises on the grounds of their main medical centers,
Comment – Hospitals play an important role in promoting healthy lifestyles among their patients, visitors, and employees. However, hospitals are also businesses that need to address important economic issues such as customer satisfaction, employee retention, and financial viability. These roles unfortunately can occasionally lead to conflicting institutional goals. During the 1980s, for example, hospitals struggled with whether to let visitors or employees smoke cigarettes within their facilities. Ultimately, hospitals decided that the benefit of allowing individuals the freedom to smoke was outweighed by their responsibility for advocating health promotion.7
Of course, fast food restaurants are not solely responsible for the rising incidence of obesity in the United States. However, their ubiquitous presence undoubtedly contributes to the proliferation of high-fat and high-calorie diets among Americans.8 Hospitals may wish to revisit the idea of serving high-calorie fast food in the very place where they also care for the most seriously ill.
(4) http://www.yaleruddcenter.org/resources/upload/docs/what/industry/FoodTobacco.pdf
The Perils of Ignoring History: Big Tobacco Played Dirty and Millions Died. How
Similar Is Big Food? KELLY D. BROWNELL and KENNETH E. WARNER Yale University; University of Michigan
Fast-food restaurants also can be found in the lobbies of many of the nation’s leading hospitals (Cram et al. 2007; Sahud et al. 2006), including McDonald’s franchises
in the lobbies of the Cleveland Clinic and the Children’s Hospital of Philadelphia. One study found that fifty-nine of two hundred hospitals with pediatric residencies had fast-food restaurants and that families who made outpatient pediatric visits were four times more likely to eat fast food (at any time of the day) if they visited a hospital with a fast-food restaurant (Sahud et al. 2006). Likewise, schools remain a branding and sales opportunity for the beverage industry at the same time it pledges
to protect children (e.g., American Beverage Association 2009).
(5) www.thesun.co.uk/sol/homepage/woman/health/health/2805543/Row-over-fast-food-in-hospitals.html
Row over Fatty Grub in Hospitals
A PATIENT in a wheelchair queues to order fast food from Burger King – in a HOSPITAL.
Another shocking image shows a poorly person attached to a DRIP being served the fatty grub – in a centre renowned for its heart care. Forty of England’s 170 NHS Trusts have rented space to fast food franchises including Subway, Upper Crust and Starbucks – and five more outlets are set to open.
(6) www.dailymail.co.uk/news/article-1242815/NHS-pays-patients-lose-weight–opening-fast-food-branches-IN-hospitals.html
NHS pays patients to lose weight – while opening fast food branches IN hospitals By Sara Nelson 13th January 2010
(7) www.cmaj.ca/cgi/content/full/179/3/213
CMAJ • July 29, 2008; 179 (3). doi:10.1503/cmaj.080975.
Frying up hospital cafeteria food = Yoni Freedhoff, MD* and Rob Stevenson, MD
*Medical Director, Bariatric Medical Institute, Ottawa, Ont.; Cardiologist, Saint John Regional Hospital, Saint John, NB
Michael Pollan
(8) www.nytimes.com/2009/09/10/opinion/10pollan.html
Big Food vs. Big Insurance By MICHAEL POLLAN September 9, 2009 NY Times.
Michael Pollan, a contributing writer for The Times Magazine and a professor of journalism at the University of California, Berkeley, is the author of “In Defense of Food: An Eater’s Manifesto.”
But so far, food system reform has not figured in the national conversation about health care reform. And so the government is poised to go on encouraging America’s fast-food diet with its farm policies even as it takes on added responsibilities for covering the medical costs of that diet. To put it more bluntly, the government is putting itself in the uncomfortable position of subsidizing both the costs of treating Type 2 diabetes and the consumption of high-fructose corn syrup.
There’s lots of money to be made selling fast food and then treating the diseases that fast food causes. One of the leading products of the American food industry has become patients for the American health care industry.
Obesity, Soft Drinks and Fructose – Dr Bray
(9)http://www.ncbi.nlm.nih.gov/pubmed/19956074
Curr Opin Lipidol. 2009 Dec 2.
Soft drink consumption and obesity: it is all about fructose. Bray GA.
Fructose, a component of both sucrose (common sugar) and high fructose corn syrup, should be of concern to both healthcare providers and the public.
Consumption of sugar-sweetened beverages has increased steadily over the past century and with this increase has come more and more reports associating their use with the risk of overweight, diabetes and cardiometabolic disease.
In a meta-analysis of the relationship between soft drink consumption and cardiometabolic risk, there was a 24% overall increased risk comparing the top and bottom quantiles of consumption. Several factors might account for this increased risk, including increased carbohydrate load and increased amounts of dietary fructose.
Fructose acutely increases thermogenesis, triglycerides and lipogenesis as well as blood pressure, but has a smaller effect on leptin and insulin release than comparable amounts of glucose. In controlled feeding studies, changes in body weight, fat storage and triglycerides are observed as well as an increase in inflammatory markers.
SUMMARY: The present review concludes on the basis of the data assembled here that in the amounts currently consumed, fructose is hazardous to the cardiometabolic health of many children, adolescents and adults.
High Fructose Corn Syrup Sweetener
(10) http://www.ajcn.org/cgi/content/full/79/4/537
American Journal of Clinical Nutrition, Vol. 79, No. 4, 537-543, April 2004
Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity1,2 George A Bray, Samara Joy Nielsen and Barry M Popkin
1 From the Pennington Biomedical Research Center, Louisiana State University, Baton Rouge, LA (GA, and the Department of Nutrition, University of North Carolina, Chapel Hill (SJN and BMP).
Teen Obesity and HFCS
(11) http://bestwellnessconsultant.com/2008/04/03/teen-obesity-and-high-fructose-corn-syrup-addiction-weight-gain-diabetes-heart-disease-best-of-mother-earth.aspx
Teen Obesity and High Fructose Corn Syrup
If you haven’t noticed High Fructose Corn Syrup is in a lot of stuff, it is the cornerstone of mass produced and processed food. It makes things ultra sweet and makes the shelf life of stuff very stable – try perpetual. High Fructose Corn Syrup is 20% cheaper than sugar. It’s a 4.5 BILLION dollar industry. It came to the market in the late 70’s, obesity levels at that time were stable. Now 50% of our sweeteners are HFCS derived. Per person consumption is at a 73.5 lbs PER YEAR.
The article sites a researcher George Bray, MD, professor of Clinical Obesity and Metabolism at the Pennington Biomedical Research Center at Louisiana State University who states based on the commentary above; the rise in obesity in the US can be linked to the increased use of HFCS
(12)
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2673878/?tool=pubmed
J Clin Invest. 2009 May 1; 119(5): 1322–1334. 2009 April 20.
Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans by Kimber L. Stanhope et al.
Studies in animals have documented that, compared with glucose, dietary fructose induces dyslipidemia and insulin resistance. To assess the relative effects of these dietary sugars during sustained consumption in humans, overweight and obese subjects consumed glucose- or fructose-sweetened beverages providing 25% of energy requirements for 10 weeks. Although both groups exhibited similar weight gain during the intervention, visceral adipose volume was significantly increased only in subjects consuming fructose. Fasting plasma triglyceride concentrations increased by approximately 10% during 10 weeks of glucose consumption but not after fructose consumption. In contrast, hepatic de novo lipogenesis (DNL) and the 23-hour postprandial triglyceride AUC were increased specifically during fructose consumption. Similarly, markers of altered lipid metabolism and lipoprotein remodeling, including fasting apoB, LDL, small dense LDL, oxidized LDL, and postprandial concentrations of remnant-like particle–triglyceride and –cholesterol significantly increased during fructose but not glucose consumption. In addition, fasting plasma glucose and insulin levels increased and insulin sensitivity decreased in subjects consuming fructose but not in those consuming glucose.
These data suggest that dietary fructose specifically increases DNL, promotes dyslipidemia, decreases insulin sensitivity, and increases visceral adiposity in overweight/obese adults.
(13) http://www.nutritionandmetabolism.com/content/2/1/5#B27
Fructose, insulin resistance, and metabolic dyslipidemia Heather Basciano , Lisa Federico and Khosrow Adeli
Clinical Biochemistry Division, Department of Laboratory Medicine and Pathobiology, Hospital for Sick Children, University of Toronto, Toronto, Ontario, Canada
Nutrition & Metabolism 2005, 2:5
Obesity and type 2 diabetes are occurring at epidemic rates in the United States and many parts of the world. The “obesity epidemic” appears to have emerged largely from changes in our diet and reduced physical activity. An important but not well-appreciated dietary change has been the substantial increase in the amount of dietary fructose consumption from high intake of sucrose and high fructose corn syrup, a common sweetener used in the food industry.
A high flux of fructose to the liver, the main organ capable of metabolizing this simple carbohydrate, perturbs glucose metabolism and glucose uptake pathways, and leads to a significantly enhanced rate of de novo lipogenesis and triglyceride (TG) synthesis, driven by the high flux of glycerol and acyl portions of TG molecules from fructose catabolism.
These metabolic disturbances appear to underlie the induction of insulin resistance commonly observed with high fructose feeding in both humans and animal models. Fructose-induced insulin resistant states are commonly characterized by a profound metabolic dyslipidemia, which appears to result from hepatic and intestinal overproduction of atherogenic lipoprotein particles. Thus, emerging evidence from recent epidemiological and biochemical studies clearly suggests that the high dietary intake of fructose has rapidly become an important causative factor in the development of the metabolic syndrome.
There is an urgent need for increased public awareness of the risks associated with high fructose consumption and greater efforts should be made to curb the supplementation of packaged foods with high fructose additives. The present review will discuss the trends in fructose consumption, the metabolic consequences of increased fructose intake, and the molecular mechanisms leading to fructose-induced lipogenesis, insulin resistance and metabolic dyslipidemia.
In a 2004 study, Gross et al examined nutrient consumption in the United States between 1909 and 1997, and discovered there was a significant correlation in the prevalence of diabetes with fat, carbohydrate, corn syrup, and total energy intakes. Most striking was the fact that when total energy intake was accounted for, corn syrup was positively associated with type 2 diabetes, while protein and fat were not [32].
High fructose corn syrups (HFCS) are quite commonly found in soft drinks and juice beverages, and are incorporated into many convenient pre-packaged foods, such as breakfast cereals and baked goods. Fructose consumption has thus largely increased over the past few decades most likely as a result of this increased use of HFCS, which contains between 55–90% fructose. The use of HFCS has increased an alarming 1000% between 1970 and 1990 [33]. In 1970, individual consumption of fructose was only 0.5 lb/year. However, in 1997, this figure rose to an alarming 62.4 lb/year [34]. The type of common, general use sweeteners represent as large an impact as the dramatic increase in the use of these caloric sweeteners. Between 1909 and 1997, sweetener use increased by 86%; and specifically, corn syrup sweeteners now represent over 20% of total daily carbohydrate intake, at an increase of 2100% [32].
Fructose metabolism
Fructose is readily absorbed and rapidly metabolized by human liver. For thousands of years humans consumed fructose amounting to 16–20 grams per day, largely from fresh fruits. Westernization of diets has resulted in significant increases in added fructose, leading to typical daily consumptions amounting to 85–100 grams of fructose per day. The exposure of the liver to such large quantities of fructose leads to rapid stimulation of lipogenesis and TG accumulation, which in turn contributes to reduced insulin sensitivity and hepatic insulin resistance/glucose intolerance. These negative effects of fructose are the reason that fructose metabolism has gained recent research attention
In 1992, the USDA recommended that only 40 g of extra sugars should be added to a standard 2000 calorie a day diet [35]. The amount of HFCS found in only one 12-oz soft drink equals this total proportion of daily intake.
In the liver, fructose is metabolized into glyceraldehyde and dihydroxyacetone phosphate. These particular fructose end products can then readily converge with the glycolytic pathway. Of key importance is the ability of fructose to by-pass the main regulatory step of glycolysis, the conversion of glucose-6-phosphate to fructose 1,6-bisphosphate, controlled by phosphofructokinase. Thus, while glucose metabolism is negatively regulated by phosphofructokinase, fructose can continuously enter the glycolytic pathway. Therefore, fructose can uncontrollably produce glucose, glycogen, lactate, and pyruvate, providing both the glycerol and acyl portions of acyl-glycerol molecules. These particular substrates, and the resultant excess energy flux due to unregulated fructose metabolism, will promote the over-production of TG
The increasing application of high fructose sweeteners over the past few decades has resulted in a considerable rise in the dietary intake of fructose. A high flux of fructose to the liver, the main organ capable of metabolizing this simple carbohydrate, disturbs normal hepatic carbohydrate metabolism leading to two major consequences (Figure 2): perturbations in glucose metabolism and glucose uptake pathways, and a significantly enhanced rate of de novo lipogenesis and TG synthesis, driven by the high flux of glycerol and acyl portions of TG molecules coming from fructose catabolism. These metabolic disturbances appear to underlie the induction of insulin resistance commonly observed with high fructose feeding in both humans and animal models.
Fructose induced insulin resistant states are commonly characterized by a profound metabolic dyslipidemia, which appears to result from hepatic and intestinal overproduction of atherogenic lipoprotein particles.
In conclusion, emerging evidence from recent epidemiological and biochemical studies clearly suggests that the high dietary intake of fructose has rapidly become an important causative factor in the development of the metabolic syndrome. There is an urgent need for increased public awareness of the risks associated with high fructose consumption and greater efforts should be made to curb the supplementation of packaged foods with high fructose additives.
(14) http://ddr.nal.usda.gov/dspace/bitstream/10113/22238/1/IND44124650.pdf
Br J Nutr. 2008 Nov;100(5):947-52.
Consumption of fructose-sweetened beverages for 10 weeks increases postprandial triacylglycerol and apolipoprotein-B concentrations in overweight and obese women.
Swarbrick MM, Stanhope KL, Elliott SS, Graham JL, Krauss RM, Christiansen MP, Griffen SC, Keim NL, Havel PJ.
Department of Nutrition, University of California, Davis, CA 95616, USA.
The objective of the present study was to investigate the metabolic effects of 10-week consumption of fructose-sweetened beverages in human subjects under energy-balanced conditions in a controlled research setting. Following a 4-week weight-maintaining complex carbohydrate diet, seven overweight or obese (BMI 26.8-33.3 kg/m2) postmenopausal women were fed an isoenergetic intervention diet, which included a fructose-sweetened beverage with each meal, for 10 weeks. The intervention diet provided 15 % of energy from protein, 30 % from fat and 55 % from carbohydrate (30 % complex carbohydrate, 25 % fructose).
Fasting and postprandial glucose, insulin, TAG and apoB concentrations were measured. Fructose consumption increased fasting glucose concentrations and decreased meal-associated glucose and insulin responses (P = 0.0002, P = 0.007 and P = 0.013, respectively).
Moreover, after 10 weeks of fructose consumption, 14 h postprandial TAG profiles were significantly increased, with the area under the curve at 10 weeks being 141 % higher than at baseline (P = 0.04). Fructose also increased fasting apoB concentrations by 19 % (P = 0.043 v. baseline). In summary, consumption of fructose-sweetened beverages increased postprandial TAG and fasting apoB concentrations, and the present results suggest that long-term consumption of diets high in fructose could lead to an increased risk of CVD.
Fructose and Hypertension
(15)
http://hyper.ahajournals.org/cgi/reprint/10/5/512
Hypertension, Vol 10, 512-516,
Fructose-induced insulin resistance and hypertension in rats
IS Hwang, H Ho, BB Hoffman and GM Reaven
Department of Medicine, Stanford University School of Medicine, Palo Alto, California.
To determine if hypertension could be produced in normal rats by feeding them a fructose-enriched diet, Sprague-Dawley rats were fed either normal chow or a diet containing 66% fructose as a percentage of total calories for approximately 2 weeks. At the end of this period systolic blood pressure had increased from 124 +/- 2 to 145 +/- 2 (SEM) mm Hg in the fructose-fed rats, whereas no change occurred in the control group.
In addition, hyperinsulinemia and hypertriglyceridemia were associated with hypertension in fructose-fed rats.
Type 2 Diabetes Soda Pop – HFCS
(16) http://www.commercialalert.org/schultzesoda.pdf
Sugar-Sweetened Beverages, Weight Gain,and Incidence of Type 2 Diabetes in Young and Middle-Aged Women
Conclusion Higher consumption of sugar-sweetened beverages is associated with
a greater magnitude of weight gain and an increased risk for development of type 2
diabetes in women, possibly by providing excessive calories and large amounts of rapidly absorbable sugars.
(17) http://jama.ama-assn.org/cgi/content/full/292/8/927
JAMA. 2004;292:927-934 SUGAR-SWEETENED BEVERAGES AND DIABETES IN WOMEN
HFCS
(18) http://www.kitchentablemedicine.com/high-fructose-corn-syrup-sugar/
Corn Syrup, Is it Really Just Like Sugar? January 30, 2009 by Kitchen Table Medicine
FRUCTOSE ALSO:
■Creates harmful proteins, called glycated proteins, much easier than glucose.
■Leads to insulin insensitivity (and, therefore: diabetes and obesity as well).
■Contributes to hypertension (high blood pressure).
(19)
http://www.westonaprice.org/The-Double-Danger-of-High-Fructose-Corn-Syrup.html
The Double Danger of High Fructose Corn Syrup Written by Bill Sanda 2004-Feb-19
(20)http://www.lef.org/magazine/mag2008/dec2008_Metabolic-Dangers-of-High-Fructose-Corn-Syrup_02.htm
LE Magazine December 2008 Metabolic Danger of High-Fructose Corn Syrup By Dana Flavin, MS, MD, PHD
(21)http://www.timesonline.co.uk/tol/news/uk/health/article6954603.ece
December 13, 2009 Child diabetes blamed on food sweetener
(22) http://en.wikipedia.org/wiki/High-fructose_corn_syrup
High Fructose Corn Syrup Obesity
(23) http://www.sfgate.com/cgi-bin/blogs/sfmoms/detail?entry_id=55267
Corn syrup removed from SFUSD chocolate milk
(24) http://www.trit.us/modernfood/highfructose.html#author
http://www.evadeandsurvive.com/syrup
The Double Dangers of High Fructose Corn Syrup By Bill Sanda, BS, MBA
(25) http://www.slate.com/id/2216796/
Dark Sugar The decline and fall of high-fructose corn syrup. By Daniel Engber
Posted Tuesday, April 28, 2009, at 4:15 PM ET
(26) http://www.youtube.com/drinkingfat
You Tube Drinking FAT
(27) http://lowcarbdiets.about.com/od/whattoeat/a/sugars.htm
Here is a list of some of the possible code words for “sugar” which may appear on a label. Hint: the words “syrup”, “sweetener”, and anything ending in “ose” can usually be assumed to be “sugar”. If the label says “no added sugars”, it should not contain any of the following, although the food could contain naturally-occurring sugars (such as lactose in milk).
•Corn sweetener
•Corn syrup, or corn syrup solids
•Dehydrated Cane Juice
•Dextrin
•Dextrose
•Fructose
•Fruit juice concentrate
•Glucose
•High-fructose corn syrup
•Honey
•Invert sugar
•Lactose
•Maltodextrin
•Malt syrup
•Maltose
•Maple syrup
•Molasses
•Raw sugar
•Rice Syrup
•Saccharose
•Sorghum or sorghum syrup
•Sucrose
•Syrup
•Treacle
•Turbinado Sugar
•Xylose
———————–
Michael Pollen on Food Rules
(28) http://www.slashfood.com/2010/01/15/michael-pollan-on-food-rules/
Processed food is cheaper. How do you get around that? MP: That is a big challenge. The fact is, in this country, today, to eat well you need more money and that is because the system is rigged in favor of processed foods. The government subsidizes corn and soy beans, which in effect subsidizes fast food because the corn gets turned into high-fructose corn syrup and cattle and chicken feed, and the soy gets turned into the hydrogenated oil in which all fast food is fried. To make this system more equitable and to make healthy food accessible to everyone, we need to change the farm policies at a federal level and create incentives to make farmers grow real food, simple vegetables, whole grains and fruits and less attractive to grow the building blocks of fast food.
(29)
http://www.nih.gov/news/pr/dec2004/nhlbi-30.htm
Eating at Fast-food Restaurants More than Twice Per Week is Associated with More Weight Gain and Insulin Resistance in Otherwise Healthy Young Adults
(30)
http://minority-health.pitt.edu/archive/00000470/01/Fast-food_Habits,_Weight_Gain,_and_Insulin_Resistance.pdf
Fast-food Habits, Weight Gain, and Insulin Resistance (The CARDIA Study): 15-Year Prospective Analysis”. Mark Pereira, Alex I. Kartashov, Cara B. Ebbeling, Linda Van Horn, Martha L. Slattery, David R. Jacobs, Jr., David S. Ludwig. The Lancet, January 1, 2005.
Certain fast foods contain large amounts of partially hydrogenated oils, and this class of fatty acids can cause insulin resistance and increase risk of type 2 diabetes.15 Fast food also contains large amounts of highly refined starchy food and added sugar, carbohydrates that have been characterised as high in glycaemic index.28 Consumption
of a high glycaemic index or high glycaemic load diet has been linked to risk for diabetes, independent of bodyweight changes,
——————–
Cholesterol Screening and Statins in Children and Teens
CDC Report on Prevalence of Abnormal Lipid Levels
(28) http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5902a1.htm
Prevalence of Abnormal Lipid Levels Among Youths — United States, 1999–2006
Weekly January 22, 2010 / 59(02);29-33 MM Weekly Report (MMWR) CDC
In 2008, the American Academy of Pediatrics (AAP) established recommendations for targeted screening of youths aged ≥2 years for abnormal blood lipid levels (2). To provide prevalence data on abnormal lipid levels among youths, eligibility for lipid screening based on BMI, and eligibility for therapeutic lifestyle counseling among overweight youths, CDC analyzed results from the National Health and Nutrition Examination Survey (NHANES) for 1999–2006. This report describes the results of that analysis, which found that the prevalence of abnormal lipid levels among youths aged 12–19 years was 20.3%. This prevalence varied by BMI; 14.2% of normal weight youths, 22.3% of overweight and 42.9% of obese had at least one abnormal lipid level. Among all youths, 32% had a high BMI and therefore would be candidates for lipid screening under AAP recommendations. Given the high prevalence of abnormal lipid levels among youths who are overweight and obese in this study, clinicians should be aware of lipid screening guidelines, especially recommendations for screening youths who are overweight or obese.
Recommended interventions focus on dietary changes (e.g., reduced consumption of saturated fat and dietary cholesterol, and increased consumption of dietary fiber) to improve LDL-C (5,6). Weight management through an improved diet and nutritional counseling also is recommended as a primary treatment of abnormal lipid levels. Finally, studies suggest that physical activity might improve HDL-C and triglyceride levels, and to some extent, LDL-C concentrations (7). Although therapeutic lifestyle counseling is the first course of action in reducing abnormal lipid levels among youths, AAP recommends considering pharmacologic interventions to treat children whose LDL remains persistently high even after therapeutic lifestyle counseling (2).
http://pediatrics.aappublications.org/cgi/content/full/101/1/141
PEDIATRICS Vol. 101 No. 1 January 1998, pp. 141-147
AMERICAN ACADEMY OF PEDIATRICS: Cholesterol in Childhood Committee on Nutrition
http://pediatrics.aappublications.org/cgi/content/abstract/122/1/198
PEDIATRICS Vol. 122 No. 1 July 2008, pp. 198-208 (doi:10.1542/peds.2008-1349)
Lipid Screening and Cardiovascular Health in Childhood
Stephen R. Daniels, MD, PhD, Frank R. Greer, MD and the Committee on Nutrition
http://www.cspinet.org/integrity/watch/200807211.html
Pediatrics Fails to Disclose Industry Ties in Lipid Guide for Kids . . . American Academy of Pediatric’s new cholesterol guidelines for children did not reveal the industry ties of three of the six authors despite its policy requiring conflict of interest disclosure in its flagship journal. The recommendations, which appeared in the current issue of Pediatrics, caused a national uproar by recommending statin drugs for children as young as eight
http://www.cnn.com/2010/HEALTH/01/22/teens.cholesterol/
CDC: 1 in 5 teens has cholesterol problems. Now what?
By Sarah Klein, January 22, 2010 CNN News
One in five teens in the U.S. — and more than 40 percent of obese teens — have abnormal cholesterol, whether it’s low HDL (good cholesterol); high LDL (bad cholesterol); or high levels of triglycerides, another type of blood fat, according to a new report from the Centers for Disease Control and Prevention.
The findings suggest that the American Academy of Pediatrics’s (AAP) 2008 guidelines — which recommend more aggressive cholesterol testing and intervention in kids, particularly the overweight and obese — make sense, the authors conclude.
The 2008 guidelines created controversy because, for the first time, cholesterol tests were recommended for overweight or high-risk children as young as 2 years old, and treatment with a cholesterol-lowering statin was an option for children as young as 8 who had bad cholesterol, or LDL, over 190 mg/dL, and who couldn’t lower their cholesterol with diet or exercise. (The previous guidelines said children should be older than 10 before medication was considered, and statins weren’t on the list.)
Statins for kids?
Placing a child on statins is different than prescribing the medications to adults, who typically wouldn’t start a drug regimen until middle age. “If you’re going to start a 10-year-old on it and say, ‘You need to take this for the rest of your life’, there’s some doubt as to whether that would be a good idea,” says Lee. “People are a bit wary of that, because [statins are] something that could potentially affect growth and development.”
Part of it may also depend on what the doctor prefers. “Some [thought] we need to be aggressive about preventing cardiovascular disease in children,” says Lee. “Others have [questioned] the long-term side effects and [whether] we should really be prescribing this in kids.”
A more aggressive treatment may be best for certain high-risk children. Autopsy studies do suggest that the first signs of heart disease — fatty “streaks” or accumulation of plaque in arteries — show up in childhood, so screening and treating sooner may prevent complications down the road.
Doctors can prescribe statins in children with LDL, or bad cholesterol, levels of over 190 mg/dL with no other risk factors, or in children with LDL levels over 160 mg/dL with risk factors like diabetes, kidney failure, obesity, high blood pressure, or a family history of heart disease.
“Exactly what age to start is slightly controversial,” says Dr. Samuel S. Gidding, the chief of pediatric cardiology at the Alfred I. DuPont Hospital for Children, in Wilmington, Delaware. “But the earlier you treat, the likelier you are to be effective with treatment.”
Statins seem to be relatively safe, says Gidding. The benefits may outweigh the risks of giving them to children at a young age, especially if cholesterol and, therefore, heart disease risk are very high — although no one really knows what happens when children take the drugs over the course of a lifetime.
http://pediatrics.aappublications.org/cgi/content/full/122/4/904
PEDIATRICS Vol. 122 No. 4 October 2008, pp. 904-905 (doi:10.1542/peds.2008-2103)
LETTER TO THE EDITOR An Assessment of the New Lipid Screening Guidelines Michael J. Steiner, MD Wallace D. Brown, MD Department of Pediatrics Edmund Liles, MD Departments of Pediatrics and Internal Medicine University of North Carolina School of Medicine Chapel Hill, NC 27514
We do not have high-quality evidence to know whether targeted cholesterol screening will help us to address the potential impending wave of cardiovascular disease attributable in part to obesity and sedentary habits acquired in childhood.
However, the AAP should acknowledge also that because high-quality evidence is not available, a definitive screening recommendation cannot be made
http://nejm.highwire.org/cgi/content/full/359/13/1309
Volume 359:1309-1312 September 25, 2008 Number 13 NEJM
Storm over Statins — The Controversy Surrounding Pharmacologic Treatment of Children, Sarah de Ferranti, M.D., M.P.H., and David S. Ludwig, M.D., Ph.D.
http://junkfoodscience.blogspot.com/2008/07/is-it-for-real-cholesterol-screening-in.html
July 08, 2008 Is it for real? Cholesterol screening in toddlers and statins from elementary school age?
http://www.nytimes.com/2008/07/08/health/08well.html?_r=2&ref=health&oref=slogin
8-Year-Olds on Statins? A New Plan Quickly Bites Back By TARA PARKER-POPE July 8, 2008 NY Times
While some doctors applauded the idea, others were incredulous. In particular, these doctors called attention to a lack of evidence that the use of the cholesterol-lowering drugs, called statins, in children would prevent heart attacks later in life.
“What are the data that show this is helpful preventing heart attacks?” asked Dr. Darshak Sanghavi, a pediatric cardiologist and assistant professor at the University of Massachusetts Medical School. “How many heart attacks do we hope to prevent this way? There’s no data regarding that.” Nor, Dr. Sanghavi added, are there data on the possible side effects of taking statins for 40 or 50 years.
Under the old guidelines, children considered at high risk for heart disease could be given statins starting at age 10. The new guidelines apply to children as young as 8 with LDL, or “bad,” cholesterol of 190 milligrams per deciliter, or those with LDL of 160 and a family history of heart disease or two other risk factors. Among children with diabetes, drug treatment may begin when bad cholesterol reaches 130.
The report’s lead author, Dr. Stephen Daniels, told The Associated Press that he had worked as a consultant to Abbott Laboratories and Merck.
http://www.reuters.com/article/idUSTRE60K54I20100122
One-fifth of U.S. teens have unhealthy cholesterol
http://abcnews.go.com/Health/WellnessNews/test-teens-high-cholesterol/story?id=9628671
Should We Test Teens for High Cholesterol? American Teens May Be at Risk for Problems Once Associated Only With Middle Age By JOHN GEVERJan. 22, 2010 MedPage Today Senior Editor
http://www.npr.org/blogs/health/2010/01/high_cholesterol.html
For Kids With High Cholesterol, Change Diet, Exercise Before Drugs January 22, 2010 By Nadja Popovich
http://thespeckledbanana.blogspot.com/2010/01/more-business-for-big-pharma.html
Saturday, January 23, 2010 More Business for Big Pharma
Just what we needed right? It looks like with teen obesity on the rise, we’re seeing an increase in teen cholesterol levels too. It was inevitable. The U.S. Centers for Disease Control and Prevention (CDC) reported on Thursday that one in five American teens has unhealthy cholesterol levels (a major risk factor for heart disease in adults). Heart disease still remains the leading cause of death in the United States.
What does this mean? More clients for Big Pharma! I bet they’re laughing their way to the bank now. Presently, there are quite a few drugs used to control cholesterol levels in adults – so why not use them for teens too?
http://www.huffingtonpost.com/dr-michael-j-breus/statins-for-kids_b_116379.html
Statins for Kids?Dr. Michael J. Breus 10-Day Boot Camp for a Healthier Lifestyle
•Avoid processed foods, fast food, refined sugar, hydrogenated fats, and white flour. Go organic wherever possible.
•Schedule at least 30 minutes of physical exercise at least 7 of those 10 days. If you can, do 60 minutes total on your exercise days.
•Cut out all soda and juices. Opt for plain water or sparkling mineral water.
•Do not consume any caffeine after 2 p.m. in the afternoon. Minimize or avoid alcohol.
•Set strict boundaries between work and play. Avoid work within two hours of bed, including household chores, and leave one weekend day for goofing off.
•Get however much sleep you need each night to feel refreshed the next day; go to bed and rise at the same exact time each day–weekends included.
http://organizedwisdom.com/helpbar/index.html?return=http://organizedwisdom.com/Statins_for_Children&url=www.it-takes-work.com/2009/02/little-johnny-needs-a-statin/
Little Johnny Needs A Statin February 18, 2009
http://www.drhoffman.com/page.cfm/838
Statins for Kids?–A Terrible Idea Tuesday, July 8
Cholesterol Drugs for Kids Could Reduce Heart Attacks in Adulthood
Kids should get screened for cholesterol — and some as young as 8 should get cholesterol-lowering drugs. Those are the recommendations from the American Academy of Pediatrics, which today published a new set of guidelines on lipid screening (online here).
The guidelines point out that atherosclerosis — the hardening of the arteries that leads to heart disease — begins in childhood. And, they note, more than 10% of kids have total cholesterol levels over 200 mg/dL, which is “a level of concern in adults.”
For the many kids with high cholesterol who are overweight, shedding pounds should be the first course of action. Switching to reduced-fat milk after overweight kids hit 1 is also a good idea. A low-fat diet makes sense for all kids older than 2.
Kids with very high bad cholesterol, or LDL — 190 without other risk factors; 160, if other risk factors are present; 130 in kids with diabetes — should also change their diet to eat fewer saturated fats. If that doesn’t work, cholesterol lowering drugs such as statins may be appropriate.
“If we are more aggressive about this in childhood, I think we can have an impact on what happens later in life … and avoid some of these heart attacks and strokes in adulthood,” Stephen Daniels told the AP. Daniels, a Colorado pediatrician who was one of the authors of the guidelines, has consulted for Abbott and Merck, but not on matters involving their cholesterol drugs, the AP said.
Opposed to Cholesterol Screening in Kids and AAP Guidelines
http://www.glgroup.com/News/Our-Kids-on-Statins………..Not-26357.html
Our Kids on Statins………..Not! July 10, 2008
With the pipeline for new drugs running dry, it is no surprise that pharmaceutical companies are looking to expand indications for existing products still under patent protection. What better way to do this than by creating entirely new patient populations out of whole cloth?
Analysis
New guidelines from the American Academy of Pediatrics (AAP) suggesting use of statins in children with elevated LDL are nothing short of astonishing. Yes, childhood obesity and metabolic syndrome are on the rise, but where is the evidence that statin therapy will help and not harm children? Reading the NCEP ATP guidelines for treatment of hypercholesterolemia in adults is instructive. The underlying concept that elevated LDL is toxic, and that treatment of this is beneficial, permeates the entire document. Little attention is given to obvious problems with this simplistic model, such as the lack of success of early studies using non-statin cholesterol lowering agents. The bias towards treatment of otherwise healthy individuals who have elevated LDL (targets keep dropping) with statin therapy is based largely on epidemiologic data, and one flawed prospective trial (WOSCOPS).
Already, this treatment model has been extended to the elderly, many of whom will clearly not benefit. The ATP panelists have extensive industry financial relationships, that in my view, must create some bias. The AAP panelists did not list financial disclosures, but it would be interesting to see them.
We cannot extrapolate data across populations. We need at least one prospective, double blind, controlled trial of statins in children before a recommendation can be made.
Solution- Farmers Market at Hospitals
http://www.cnn.com/2009/HEALTH/06/03/farmers.markets.hospitals/index.html
Farmers markets bloom at hospitals
Corn Industry Defends HFCS
http://www.sweetsurprise.com/myths-and-facts/top-hfcs-myths
http://www.sweetsurprise.com/myths-and-facts/top-hfcs-myths/gmo-corn-hfcs
Arthur Frank, M.D., Medical Director of the George Washington University Weight Management Program talks about global obesity and HFCS.
Soda Pop Vending Machine Ban in Schools
http://departments.oxy.edu/uepi/publications/APHA_Talk.htm
SODA BANS, FARM-TO-SCHOOL, AND FAST FOOD IN HOSPITALS:
AN AGENDA FOR ACTION THE OBESITY CRISIS: CHALLENGING THE FAST FOOD CULTURE
AMERICAN PUBLIC HEALTH ASSOCIATION ANNUAL MEETING Philadelphia – November 13, 2002 ROBERT GOTTLIEB and Amanda Shaffer Henry R. Luce Professor of Urban and Environmental Policy, Director, Urban & Environmental Policy Institute
Occidental College
http://departments.oxy.edu/uepi/cfj/publications/Challenging_the_Soda_Companies.pdf
CHALLENGING THE SODA COMPANIES: THE LOS ANGELES UNIFIED SCHOOL DISTRICT SODA BAN
http://www.stateline.org/live/details/story?contentId=53584
Monday, September 12, 2005 Purging pop from the schools: Wake-up call for the states
By Neal Peirce, Special to Stateline.org
http://www.dcmsonline.org/jax-medicine/2007journals/ChildhoodObesity/softdrinks.pdf
How Soft Drinks Contribute to the Pediatric Obesity Epidemic
Jonathan R. Ramprasad, MD and Jonathan S. Evans, MD
Northeast Florida Medicine Vol. 58, No. 4 2007 25
Ban Cigarette Smoking in Hosptials
http://jama.ama-assn.org/cgi/content/summary/253/20/2999
Reducing Smoking in Hospitals A Time for Action
Anthony M. H, Ho, MS, PE, MD JAMA. 1985;253(20):2999-3000.
THE FACT that cigarette smoking is widespread in hospitals is a paradox. Smoking, voluntary and involuntary, is a major risk factor associated with respiratory and cardiovascular disease, a growing list of malignancies,
GMO and HFCS
http://gmo-watch.com/pages/hfcs.asp
High-fructose corn syrup. Although HFCS is not a GMO product per se, so much HFCS is made using GM corn, we think its inclusion into these pages is justified. HFCS is widely suspected of being one of the culprits behind the obesity explosion in the United States and elsewhere during the last twenty or so years.
Fecal Bacteria in Soda Fountains at the Fast Food Restaurant
http://www.cnn.com/2010/HEALTH/01/08/soda.fountain.bacteria/index.html
Soda fountains contained fecal bacteria, study found By Madison Park, CNN January 8, 2010 6:35 p.m. EST
http://www.ncbi.nlm.nih.gov/pubmed/19926155
Beverages obtained from soda fountain machines in the U.S. contain microorganisms, including coliform bacteria . Amy S. White, Renee D. Godard, Carolyn Belling Department of Biology, Hollins University, Roanoke VA, 24020, USA – International Journal of Food Microbiology Volume 137, Issue 1, 31 January 2010, Pages 61-66
crystalline fructose
http://www.thefitshack.com/2007/04/26/23-health-drinks-that-contain-crystalline-fructose/
The biggest reason this particular molecule is so bad is because of the products it is being placed in: health drinks. Vitamin Water seems to be the most popular of the beverages, but other examples are FUZE, Mistic, SoBe, Snapple and W20 for Women.
1. Cytomax Sport Drink
2. FUZE HEALTHY INFUZIONS
3. FUZE Slender Energy
4. FUZE Vitalize
5. Vitamin Water
6. HYDRIVE Energy Drink
7. Inko’s White Tea Energy
8. IQ H2O
9. Mistic RE
10. SoBe Essential Energy
11. W2O For Women
12. NutriSoda
13. Aloe’ha Drink Products
14. Function Drinks
15. Huracan Energy Drink
16. Iron Energy
17. Juici Sparkling Beverage
18. Multi-Vitamin Enhanced Water [Kiwi-Strawberry]
19. Snapple Red Tea
20. Speedo Sportswater
21. Trek Hydrator
22. Wild Waters
23. Cal-C
The body doesn`t handle large amounts of fructose well. You can maintain life with intravenous glucose, but not with intravenous fructose; severe derangement of liver function results. There is also evidence that a high intake of fructose elevates levels of circulating fats (serum triglycerides), increasing the risk of heart disease …”
Our cells use glucose for energy by metabolizing carbohydrates. With glucose from cane or beet sugar, 20% is passed onto the liver to be metabolized. But the gut doesn`t know what to do with isolated high fructose. So it passes 100% of the isolated fructose into the liver.
Consequently, the liver metabolizes the high fructose content into mostly fats and triglycerides. High amounts of HFCS are apt to create non alcoholic fatty liver disease (NAFLD), and possibly cirrhosis. Insulin resistance is another manifestation of HFCS metabolic damage.
Sugar is a Drug leading to Addiction
http://www.radiantrecovery.com/newsensitive6.htm
The scientific evidence of sugar addiction, Kathleen DesMaisons, Ph.D. is the best selling author of Potatoes Not Prozac, The Sugar Addict’s Total Recovery Program, Your Last Diet, Little Sugar Addicts and Your Body Speaks. Radiant Recovery® is an internet-based, international community dedicated to healing unbalanced sugar sensitivity.
http://www.lurj.org/article.php/vol1n1/sugar.xml
The Reclassification of Sugar as a Drug – Marie-Hélène Lyle: The Reclassification of Sugar as a Drug. Lethbridge Undergraduate Research Journal. 2006. Volume 1 N 1.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2235907/
Neurosci Biobehav Rev. 2008; 32(1): 20–39. Published online 2007 May 18.
Evidence for sugar addiction: Behavioral and neurochemical effects of intermittent, excessive sugar intake – Nicole M. Avena, Pedro Rada, and Bartley G. Hoebel*
http://www.ncbi.nlm.nih.gov/pubmed/12055324
Obes Res. 2002 Jun;10(6):478-88. Evidence that intermittent, excessive sugar intake causes endogenous opioid dependence. Colantuoni C, Rada P, McCarthy J, Patten C, Avena NM, Chadeayne A, Hoebel BG. Princeton University
Repeated, excessive intake of sugar created a state in which an opioid antagonist caused behavioral and neurochemical signs of opioid withdrawal. The indices of anxiety and DA/ACh imbalance were qualitatively similar to withdrawal from morphine or nicotine, suggesting that the rats had become sugar-dependent.
Jeffrey Dach MD
http://www.jeffreydach.com
http://www.drdach.com
http://www.naturalmedicine101.com
http://www.truemedmd.com
Disclaimer click here: www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship. Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Link to this article:Selling Sickness in the Lobby, Fast Food in Hospitals
http://jeffreydach.com/2010/01/27/selling-sickness-in-the-lobby–fast-food-in-hospitals-by-jeffrey-dach-md.aspx
Copyright (c) 2010,11 Jeffrey Dach MD All Rights Reserved. This article may be reproduced on the internet without permission, provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.
newCodeYorik April 17, 2015 at 1:14 PM
Many years ago I used to get my testosterone replacement injections at the local Endocrine and Diabetes Center. Every Friday at noon the center had a mandatory education and training session for the staff, and as I was leaving the Pizza Hut delivery man was arriving with a dozen pizzas and Coke for the training class. I remarked on this to the nurses all the time, who agreed it was probably hypocritical, but the consensus was that 1) most of the people who worked there were pretty healthy already, and 2) it gets people to come to the training sessions. I still thought it pretty sad.
Bridge Dale April 20, 2021 at 4:42 AM
I am seriously against the sale of fast food in hospitals. As we know, fast food is awful for your health, and selling it to sick patients will only make matters worse.