 The Unreliable TSH Lab Test
The Unreliable TSH Lab Test by Jeffrey Dach MD
This article is part one of a series, click here for part two,and click here for part three.
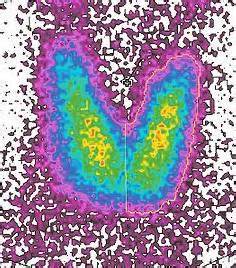
Suzy is a 59 year old post menopausal woman with low thyroid function. About three months ago, she started her bio-identical hormone program which included natural thyroid pills. After starting the program, she was doing well with more energy, better sleep, improved appearance of skin and hair, and resolution of her menopausal symptoms of flashes and sweats. However about 12 weeks into her program, Suzy had a visit with her primary care doctor who did a follow up thyroid panel. Her primary care doctor informed Suzy that her TSH test result was below the lab normal range, and therefore, her thyroid dose was too high, and should be reduced. (Note: TSH is Thyroid Stimulating Hormone, and is made by the pituitary gland). Above left image: Thyroid scan courtesy of wikimedia commons.
Suzy called me at the office distraught and confused. Two doctors were telling her two different things and she didn’t know who to believe. Her primary care doctor was telling her one thing and I was telling her another. I explained to Suzy that her primary care doctor was incorrect in relying slavishly on the TSH test. Even though her TSH test was 0.15 which is below the lab reference range of 0.3, this was perfectly acceptable and indicated her thyroid medicine was suppressing the TSH to a low level which was perfectly fine. This test interpretation means she is taking thyroid pills, and the pills are working. It does not mean she is “hyperthyroid” by any stretch of the imagination.
I also informed Suzy that her Primary Care Doctor is mistakenly relying on the TSH test to determine her thyroid dosage. The TSH test is an indirect measure of thyroid function and can be unreliable to monitor thyroid dosage. A more accurate indicator of thyroid function is the free T3, which in her case was 375, well within the normal range of 240 to 420. The Free T3 lab test together with the absence of any signs or symptoms of thyroid excess indicates she is using the correct dosage of natural thyroid medication. Symptoms of thyroid excess are rapid heartbeat or palpitations, and Suzy reported no such symptoms. In fact, Suzy said she felt fine and now that she understands it, she didn’t want to go back to feeling tired, sluggish as before she started the thyroid pills. Suzy was relieved to find out that the low TSH result was perfectly acceptable and there was nothing to worry about. This TSH scenario is a recurring event at my office.
 Conventional primary care doctors use an older thyroid lab panel which does not include the Free T3 test, the most informative thyroid lab test. Instead, mainstream endocrinology relies on the TSH test which is not a direct measure of thyroid function, and can, in fact, be unreliable.
Conventional primary care doctors use an older thyroid lab panel which does not include the Free T3 test, the most informative thyroid lab test. Instead, mainstream endocrinology relies on the TSH test which is not a direct measure of thyroid function, and can, in fact, be unreliable.
Above Left image: Thyroid Gland Anatomy Diagram, courtesy of National Institute of Health, and wikimedia commons.
Most conventional doctors are unfamiliar with the use of natural thyroid which contains both T3 and T4, and instead use Synthroid which is quite different, containing only T4. Since the Primary care doctors bill the health insurance for the office visit and payment is only a few dollars, the office visit is brief, 3-5 minutes. In this short time, Primary care doctors can provide only the most basic care, which is a quick look at the TSH lab test. If the TSH is below the lab reference range the doctor gives a new prescription for Synthroid with a reduced dosage. If the TSH is above the reference range, the primary care doctor will increase the Synthroid dosage.
 A few months ago, I found myself talking on the phone with an endocrinologist at the Cleveland Clinic explaining why the TSH blood test can be unreliable. He informed me I was wrong, and that he uses the TSH test as the gold standard. We agreed to disagree and parted company as friends. I have found that, in general, endocrinologists and mainstream doctors rely heavily on TSH to make a diagnosis of low thyroid.
A few months ago, I found myself talking on the phone with an endocrinologist at the Cleveland Clinic explaining why the TSH blood test can be unreliable. He informed me I was wrong, and that he uses the TSH test as the gold standard. We agreed to disagree and parted company as friends. I have found that, in general, endocrinologists and mainstream doctors rely heavily on TSH to make a diagnosis of low thyroid.
I recommend to you a book by Barry Durrant Peatfield, Your Thyroid and How to Keep It Healthy(1) After serving as a general practitioner in the British National Health Service, Peatfield traveled to the US to train at the Broda Barnes Institute. Peatfield later returned to England to start his own thyroid clinic. His book was written at the end of his career and contains the wisdom of 25 years of diagnosing and treating thyroid conditions. One section of the book is devoted to this question. Here it is quoted from the book: :
1) Anxiety in the medical establishment about rules and dogma has led to a slavish reliance on blood tests, such as the TSH, which are often unreliable and can actually produce a false picture.
2) Very few doctors can accept the fact that a normal, or low TSH, may still occur with low thyroid function.
3) As a result of this test (TSH), thousands are denied treatment for low thyroid condition.
After a lifetime of work serving his community, you might imagine the honors and accolades for such a knowledgeable thyroidologist as Dr Peatfield, yet quite the opposite happened. Dr. Peatfield’s license was suspended in 2001 at the age of 68 by the General Medical Council of England.(5-6) The GMC ruling was based on “unfavorable testimony” from competing endocrinologists who “slavishly rely on the TSH test” as a measurement of thyroid function to diagnose the low thyroid condition and monitor treatment with thyroxine. Sadly, this is the sort of “Witch Hunt “which has kept medical science in the “Dark Ages” regarding the treatment of the low thyroid condition.(13)
Another useful book recommended to you is written by Broda Barnes MD on the low thyroid condition. Broda Barnes MD reported 40 years ago on the same problem of his medical colleagues relying too heavily on thyroid blood tests. The book, Hypothyroidism: The Unsuspected Illnessby Barnes, Broda is a medical classic and should be required reading for every medical student and doctor. (2) I have read the book many times. The book contains the condensed wisdom of a lifetime of research and clinical experience with the thyroid, and it rings true today as it did in 1976. Thyroid blood tests come and go, yet human physiology remains the same.
Important Point: The TSH test is unreliable for determining optimal thyroid dosage. A “below lab range” TSH is routinely encountered when patients are optimally treated with natural thyroid medication and obtain the best clinical results.
Broda Barnes estimated that up to 40% of the population suffers from a low thyroid condition and would benefit from thyroid medication. Of course, Barnes’ opinion differed with that of mainstream medicine of his time which relied dogmatically on thyroid blood tests to make the diagnosis of low thyroid. Barnes felt the blood tests were unreliable and instead used the basal temperature, history and physical examination. This medical debate regarding unreliability of thyroid blood testing continues today. (3,4)
Being an astute clinician, Dr. Barnes makes a number of observations about the low thyroid condition. Firstly, low thyroid is associated with a reduced immunity to infectious diseases such as TB (tuberculosis). Before the advent of modern antibiotics in the 1940’s, most low thyroid children succumbed to infectious diseases before reaching adulthood. Secondly, low thyroid is associated with a peculiar form of skin thickening called myxedema which causes a characteristic appearance of the face, puffiness around the eyes, fullness under the chin, loss of outer eyebrows, and hair thinning or hair loss.
A third observation by Dr. Barnes is that low thyroid is associated with menstrual irregularities, miscarriages and infertility. Barnes treated thousands of young women with thyroid pills which restored cycle regularity and fertility. In his day, the medical system resorted to the drastic measure of hysterectomy for uncontrolled menstrual bleeding. Although today’s use of birth control pills to regulate the cycles is admittedly a far better alternative, Barnes found that the simple administration of desiccated thyroid served quite well. Again, Barnes noted that blood testing was usually normal in these cases which respond to thyroid medication.
A lengthy chapter is devoted to heart attacks and the low thyroid condition. Based on autopsy data from Graz Austria, Barnes concluded that low thyroid patients who previously would have succumbed to infectious diseases in childhood go on years later to develop heart disease. Barnes also found that thyroid treatment was protective in preventing heart attacks, based on his own clinical experience. Likewise for diabetes, Dr. Barnes found that adding thyroid medication was beneficial at preventing the onset of vascular disease in diabetics. Again, blood tests are usually normal.
Important Point: A low thyroid condition is a serious risk factor for heart disease.
Dr. Barnes devotes separate chapters in the book to discussion of chronic fatigue, migraine headaches and emotional/behavioral disorders all of which respond to treatment with thyroid medication.
The final chapter describes Dr. Barnes work on obesity when he presided over a hospital ward of volunteer obese patients, and monitored everything they ate. He found that the obese patients invariably ate a high carbohydrate diet, and avoided fat. Barnes added fat back into the menu and reduced the refined carbohydrates and found that his obese patients lost 10 pounds a month with no hunger pangs.
Missing from the book are discussions of Iodine supplementation and the role of the Adrenal, both of which are covered in later updated versions of Barnes thyroid book by other authors. See Hypothyroidism Type Two by Mark Starr, and Your Thyroid by Barry Durrant Peatfield. Iodine supplementation is covered by both Derry and Brownstein. The Safe Uses of Cortisol by William McK Jefferies is the companion medical classic devoted to the adrenals and cortisol.
Although Broda Barnes has since passed away, his work lives in at the Broda Barnes Institute. Patricia Puglio is the director and a great resource. She is available by phone to answer questions and offer suggestions. Here is her contact information: Patricia A. Puglio, Director, Broda O. Barnes, M.D. Research Foundation, Inc. PO Box 110098 Trumbull, CT 06611.
Thanks to Jonathan Wright’s newsletter for bringing to my attention a recent article in the June 2010 International Journal of Clinical Practice by Dr. O’Reilly which summarizes the medical literature on this question of the reliability of the TSH test. (9) Essentially, Dr O’Reilly reviews the medical literature and the history thyroid medicine and provides all the medical studies and information showing that Dr Barnes and Dr Peatfield were right all along. (7-12). Here are a few quotes from Dr O’Reilly (9):
The use of the TSH measurement to assess thyroid status in patients on thyroxine (Synthroid) replacement could be considered a classic example of the misapplication of a laboratory test.”
Instead of the TSH measurement, Dr. O’Reilly recommends the T3 test for monitoring treatment with thyroid medication. He says:
“The adequacy of thyroxine (Synthroid) replacement should be assessed clinically with the serum T3 being measured, when required, to detect over-replacement”
In spite of the obvious need for a better approach to the low thyroid condition, there has been very little movement to rehabilitate mainstream endocrinology which dogmatically clings to the TSH test and synthetic T4 only medications (levothyroxine). Here in the state of Florida, we are fortunate that the state legislature passed a Health Freedom Law in 2001. This “Health Freedom Law” protects doctors and patients from unwarranted abuse or harassment for utilizing “outside of mainstream medical practices”, such as correct diagnosis and treatment of the low thyroid condition based on the wisdom of Drs Broda Barnes, Barry Peatfield, DS O’Reilly, Jonathan Wright, David Brownstein and many others. (14)
This article is part one of a series, click here for part two,and click here for part three.
Articles with Related Interest
References and Links,
(1) Your Thyroid and How to Keep It Healthyby Durrant-Peatfield (2006). Hammersmith Press, London
(2) Hypothyroidism: The Unsuspected Illnessby Barnes, Broda Otto (1976). Harper Collins.
(3) http://ccpd.ucsf.edu/hypothyroidism.shtml Pituitary 101, UCSF California Center for Pituitary Disorders at UCSF. Web Site: “TSH is often an unreliable measure of secondary hypothyroidism and should not be used to assess the adequacy of thyroid replacement in these patients. The inappropriate use of TSH levels to determine hormone replacement is one of the more common mistakes that we see in the patients we follow, and patients should be cautious if another physician discusses changing their thyroid hormone dose. Many patients have returned for their one-year follow-up visits having had their doses lowered in response to “low TSH levels.” Most of them feel poorly, but improve after we increase or restart their medication.”
(4) http://www.bmj.com/cgi/content/full/326/7398/1087 BMJ 2003;326:1087 (17 May) Letter- Thyroid function tests and hypothyroidism, A D Toft.
“We have long taken the view that most hypothyroid patients are content with a dose of thyroxine that restores serum concentrations of thyroid stimulating hormone to the low normal range. However, some achieve a sense of wellbeing only when serum thyroid stimulating hormone is suppressed, when we take care to ensure that serum tri-iodothyronine is unequivocally normal. Until valid evidence shows that such a policy is detrimental we will continue to treat patients holistically rather than insist on adherence to a biochemical definition of adequacy of thyroxine replacement. The issue of whether a little too much thyroxine is dangerous is likely to evaporate when appropriate preparations become available to allow treat.
(5) http://www.drlowe.com/news/drpeatfield/jclletter.htm
In Defense of Dr. Barry Peatfield, letter sent ot Geneeral medical council of England as testimony on behalf of Dr. Barry Peatfield. April 17, 2001 by Dr. John C. Lowe
(6) http://news.bbc.co.uk/2/hi/health/1332644.stm
Thursday, 17 May, 2001 UK Investigation into thyroid doctor. GP Dr Barry Durrant-Peatfield, 64, who has a practice in Purley, Surrey, has been stopped from working for 18 months so that the GMC can complete its investigation.
(7) http://www.ncbi.nlm.nih.gov/pubmed/8200938 J Clin Endocrinol Metab. 1994 Jun;78(6):1368-71. Comparison of second and third generation methods for measurement of serum thyrotropin in patients with overt hyperthyroidism, patients receiving thyroxine therapy, and those with nonthyroidal illness. Franklyn JA, Black EG, Betteridge J, Sheppard MC. “Undetectable TSH results, even in a third generation assay, are not diagnostic of overt hyperthyroidism, but are also found in subjects with treated thyroid disease and NTI.”
(8) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1341585/
Br Med J (Clin Res Ed). 1986 September 27; 293(6550): 808–810. Are biochemical tests of thyroid function of any value in monitoring patients receiving thyroxine replacement? W D Fraser, E M Biggart, D S O’Reilly, H W Gray, J H McKillop, and J A Thomson. “These measurements are therefore of little, if any, value in monitoring patients receiving thyroxine replacement. “
(9) http://www.ncbi.nlm.nih.gov/pubmed/20584231
Int J Clin Pract. 2010 Jun;64(7):991-4. Thyroid hormone replacement: an iatrogenic problem.O’Reilly DS.
“Thyroid hormone replacement is one of the very few medical treatments devised in the 19th century that still survive. It is safe, very effective and hailed as a major success by patients and clinicians. Currently, it is arguably the most contentious issue in clinical endocrinology. The current controversy and patient disquiet began in the early 1970s, when on theoretical grounds and without proper assessment, the serum thyrotropin (TSH) concentration was adopted as the means of assessing the adequacy of thyroxine replacement. The published literature shows that the serum TSH concentration is a poor indicator of clinical status in patients on thyroxine. The adequacy of thyroxine replacement should be assessed clinically with the serum T3 being measured, when required, to detect over-replacement.”
(10) http://www.ncbi.nlm.nih.gov/pubmed/3122632
Ann Clin Biochem. 1987 Nov;24 ( Pt 6):614-9. Thyroid stimulating hormone measurement by an ultrasensitive assay during thyroxine replacement: comparison with other tests of thyroid function. Wheatley T, Clark PM, Clark JD, Raggatt PR, Edwards OM. “A suppressed serum TSH was found in 65% of patients with a normal serum total thyroxine. “
(11) http://www.bmj.com/content/320/7245/1332.extract
BMJ 320 : 1332 doi: 10.1136/bmj.320.7245.1332 (Published 13 May 2000) Education and debate: Thyroid function tests—time for a reassessment. Denis StJ O’Reilly, consultant clinical biochemist
(12) http://www.bmj.com/content/320/7245/1332.extract/reply#bmj_el_8954
Thyroid function tests—time for a reassessment Denis StJ O’Reilly BMJ 2000;320:1332-1334
Claims of witch-hunt as doctor is suspended for alternative thyroid care By Michael Durham Friday, 18 May 2001. Independent UK
(14) http://laws.flrules.org/2001/116
State of Florida Health Freedom Law: CHAPTER 2001-116 Senate Bill No. 1324 An act relating to health care; creating s. 456.41, F.S.; amending s. 381.026, F.S.; Ch. 2001-116 (S.B. 1324) Authorizes provision of and access to complementary or alternative health care treatments; requires specified disclosures by the health care practitioner and the keeping of certain records; conforms the Florida Patient’s Bill of Rights. Effective May 31, 2001.
Jeffrey Dach MD
7450 Griffin Road, Suite 190
Davie, Fl 33314
954-792-4663
www.jeffreydach.com
www.drdach.com
www.naturalmedicine101.com
www.bioidenticalhormones101.com
www.truemedmd.com
Click Here for: Dr Dach’s Online Store for Pure Encapsulations Supplements
Click Here for: Dr Dach’s Online Store for Nature’s Sunshine Supplements
Web Site and Discussion Board Links:
jdach1.typepad.com/blog/ disc.yourwebapps.com/Indices/244124.html
disc.yourwebapps.com/Indices/244066.html
disc.yourwebapps.com/Indices/244067.html
disc.yourwebapps.com/Indices/244161.html
disc.yourwebapps.com/Indices/244163.html
Disclaimer click here: www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship. Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Link to this article:http://wp.me/P3gFbV-Fm
Copyright (c) 2011-2013 Jeffrey Dach MD All Rights Reserved. This article may be reproduced on the internet without permission, provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.
- Jeffrey Dach MD August 1, 2013 at 9:00 AM
[…] The Unreliable TSH Lab Test by Jeffrey Dach MD […]