Decision to Start Statin Based on Calcium Score
by Jeffrey Dach MD
Have you ever wondered why statin drugs seem to be effective for secondary prevention, (people with known heart disease), and not effective for primary prevention (people without heart disease)? A new study by Joshua Mitchell explains why. Current practice dictates that Cardiologists prescribe statin drugs based on a cholesterol over 200. This has been changed by the Joshua Mitchell study from the Walter Reed Registry which supports a new decision tree. Instead of using the serum cholesterol level, the decision to give a statin drug should be based on the Calcium Score obtained from CAT scan cardiac imaging.
Calcium Score Has Replaced the Cholesterol Panel
The chart below shows that for a Calcium score of 0 to 100, there is no benefit for taking a statin drug. For a score above 100, however, the chart shows considerable reduction in MACE (major adverse cardiac event) for the statin users. Notice cholesterol level is not mentioned in this study.
Pleotropic Effects of Statin Drugs
The Joshua Mitchell study does something else. By ignoring serum cholesterol level in the decision to prescribe a statin drug, the study supports the idea that statin drug benefits are entirely due to Pleotropic effects (anti-inflammatory and antimicrobial), not due to cholesterol lowering. This is further supported by the fact that other non-statin drugs fail to have any impact on cardiovascular events. The latest was the CETP Inhibitor, Evacetrapib which lowers LDL-Cholesterol, yet failed to prevent cardovascular events compared to placebo in clinical trials, and was abandoned.(11)(Lincoff,2017) This is also true for all other non-statin cholesterol lowering drugs. They are all failures. This strongly supports the idea that all of the benefits of statin drugs are due to pleotropic effects, none from cholesterol lowering, which, in actuality, represents a liablity which impairs health.
Anti-Inflammatory Effects of Statins
As we all know, statin drugs were initially developed as cholesterol lowering agents. However, only later it was observed they had other anti-inflammatory and anti-microbial properties. For example, studies done on sepsis and pneumonia patients showed that those on statins enjoyed improved survival. (7) (Hennessy,2016) Two separate studies show patients on statins undergoing cardiac bypass surgery had reduction in peri-operative mortality by 50-70%. (5,6) (Curtis 2017) (Barakat 2016)
In-vitro studies of statin drugs show the exact mechanism of anti-inflammatory effects. Statin drugs suppresses LPS signaling in monocytes .(8)(Patel,2004) Statin drugs blocks LPS -Release of IL-6 and TNF-Alpha and decreases Nuclear Factor-KappaB.(9) (Devaraj,2006) Statin drugs prevents TNF-Alpha-Induced NF-KappaB activation and gene transcription in cultured endothelial cells.(10)(Hölschermann, 2006)
Antimicrobial Effects of Statin Drugs
Dr Emma Hennessy summarizes the research, (in vitro, cell culture and in vivo), suggesting statins could be repurposed as an anti-microbial drugs.(7) There is even efficacy against biofilm. (7)
The Power of Zero
The Joshua Mitchell study, Coronary artery calcium myocardial infarction from JACC Card Imaging 2018, is a retrospective study. Nine years of records were analyzed for 13,644 patients from the Walter Reed Army Medical Center (mean age 50 years; 71% men).
Dr Joshua Mitchell concluded: “the presence and severity of CAC (Coronary Artery Calcium) identified patients most likely to benefit from statins for the primary prevention of cardiovascular diseases.”
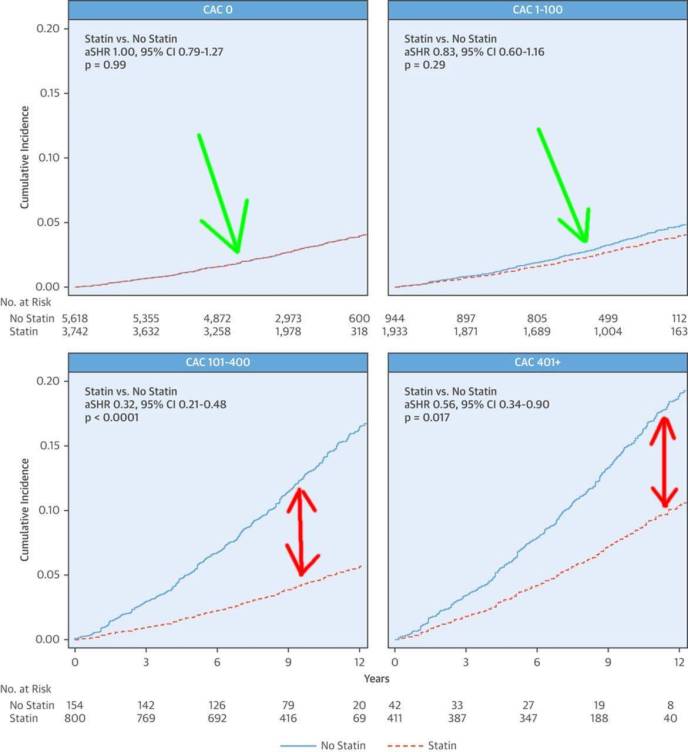
Above chart, upper panels, shows no benefit for statin drug for Calcium Score of Zero to 100 (Green Arrows) Both Statin user and non-user lines are super-imposed. Bottom two panels: For Calcium Score over 100, statin user line is nicely separated from non-statin user (Red Arrows) indicating reduction in Major Adverse cardiac Events (MACE) Statin user dotted red line.
Dr. Joshua Mitchell’s study explains why statin drugs are more effective in secondary prevention than in primary prevention of heart disease. Secondary prevention studies are in patients with known underlying heart disease and are more likely to have calcium score over 100, where statin drugs show a benefit in reducing MACE (major adverse events). Primary prevention studies are in the healthy patient population with no underlying heart disease. These patients are more likely to have a zero or low calcium score. In Zero Score patients, statin drugs provide no benefit.
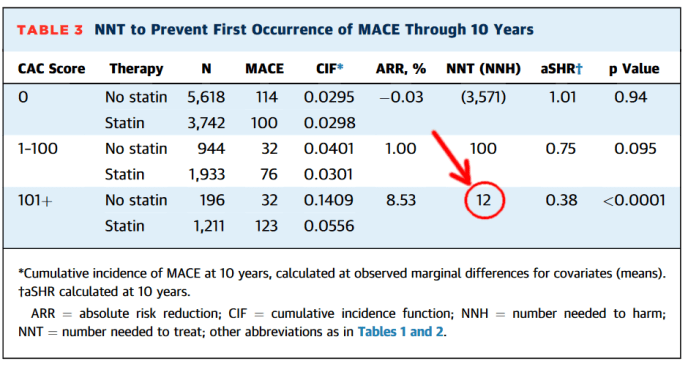
Above chart : Table 3 courtesy of Joshua Mitchell (2) Notice NNT (Number Needed to Treat) for calcium score greater than 100 drops to 12 (red arrow and red circle). Note:This is over ten years of treatment, however.
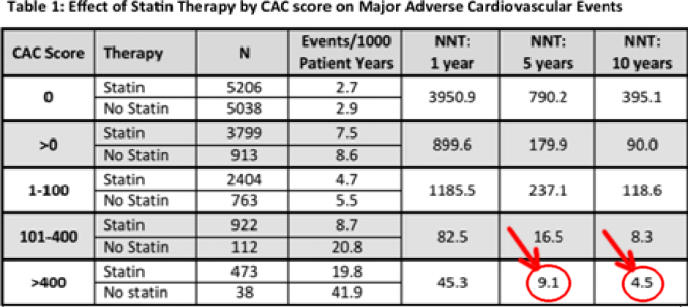
Above chart: Table 1 from abstract shows for Calcium score over 400, NNT drops to 4.5 for 10 years on statin drug. (red arrow and red circle) Courtesy of Joshua Mitchell (4)
Adverse Effects of Statin Drugs
Granted, using calcium score to determine who to treat with a statin drug allows refinement of the NNT (Number Needed to Treat) down to 4.5 over 10 years for those with calcium score over 400. However what are the adverse side effects? This is an important question. How many of these long term statin users end up in wheel chairs unable to walk because of statin induced myopathy. How many suffer from debilitating neuropathy, cognitive dysfunction and dementia? Are we trading away quality of life to buy a reduction in cardiac events? Many practitioners would argue adverse side effects are so severe, it would be preferable to avoid statins and reduce calcium score with alternative methods.
Statins Accelerate Progression of Calcium Score
Another disturbing finding is that statin drugs actually accelerate progression of calcium score according to Dr. Dykun in the 2016 Heinz Nixdorf Recall study. (15) Based on the 2004 Paolo Raggi data, annual progression of calcium score higher than 15% is a bad omen, predictive for heart attack within a few years in about 8-9% of the 500 patients on statin drugs Dr Raggi followed for 6 years.. However, for the other 450 (91%) patients on statin drugs, the calcium score progression was less than 15%, and these patients enjoyed a benign prognosis. Remarkably in the non-progressor group, the higher baseline calcium score people, above 1000, enjoyed the same benign prognosis as the lower score people (0-100). (See chart below)
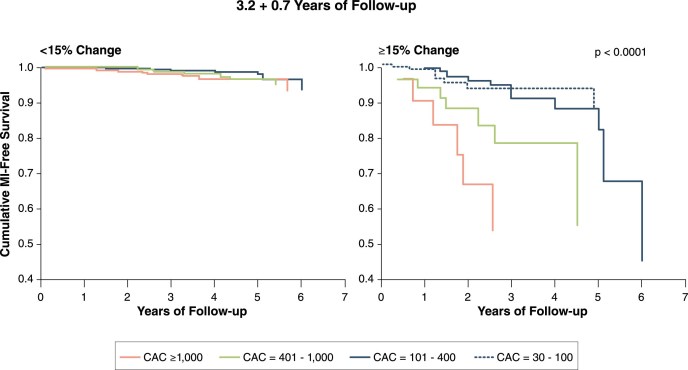
Above image courtesy of Paolo Raggi 2004.(16,17) All patients on statin drugs. Left Chart are Non-Progressors, less than 15% annual increase in calcium score showing good prognosis, all lines converge at top of chart. Right Chart: These are the Progressors with Greater than 15% annual progression of calcium score. Chart shows graded separation according to baseline calcium scores with more rapid decline to MI for higher scores.(17)
The Statin Drug Doesn’t Help the Progressors
Notice the statin drug accelerates vascular calcification in 8-9% of patients on them. See Right Chart, Progressors, Accelerated vascular calcification while on a statin drug is associated with early myocardial infarction, indicates statin drug failure, and changing to a different treatment modality is advised.
For Non-Progressors (left chart) their calcification is stable with less than 15% annual increase. They enjoy a benign prognosis.
How to Explain Statin Drug Failures?
What feature or bio-marker defines which group of patients we will fail into, Progressor or Non-Progressor in the 2004 Peolo Raggi study? How do we explain the statin drug failures, the Progressors who had MI’s in spite of the statin drug?
Obviously, cholesterol level is a useless biomarker, since it was the same for both groups. Unfortunately, the authors of the study did not comment or propose an explanation. I would propose this explanation:the defining factor is the severity of endotoxemia.
Severity of Endotoxemia, Not Cholesterol Level
I would propose the following: In the non-progressors, these people have lower levels of endotoxemia which can be successfully opposed by the pleotropic effects of the statin drug. For the Progressors, they have more severe, unrelenting endotoxemia which overwhelms the weak effects of the statin drug and leads rapidly to MI (myocardial infarction) within 6 years. We await further research to confirm this hypothesis.
Reducing Calcium Score with Aged Garlic and Essential Phospholipid
My previous article on Aged Garlic shows superiority over statin drugs for reduction in calcium score without adverse effects of statin drugs. One might argue that aged garlic together with other combined modalities such as vitamin C, Tocotrienols, Vitamin K2, Vitamin D3, Magnesium, Essential Phospholipid, Fibrinolytic Enzymes, Berberine, addressing leaky gut, eliminate wheat and other foods that cause leaky gut…etc, might prove even more effective for reducing calcium score than statin drugs, without the adverse side effects.
Perio-Odontal Disease Causes Coronary Artery Disease
Periodontal disease and other occult other infections are frequent culprits seeding endotoxemia and causing atherosclerosis.(12-14) See my previous article on the LPS Theory of Heart Disease. A visit to your local biologic dentist for a good set of dental xrays can help find the problem.
Essential Phospholipid For Reduction in Calcium Score:
My previous article discussed case material courtesy of James Roberts MD on benefits of essential phospholipid for reversing heart disease. Here is a case report courtesy of Dr. James Roberts of Toledo Ohio (below chart):
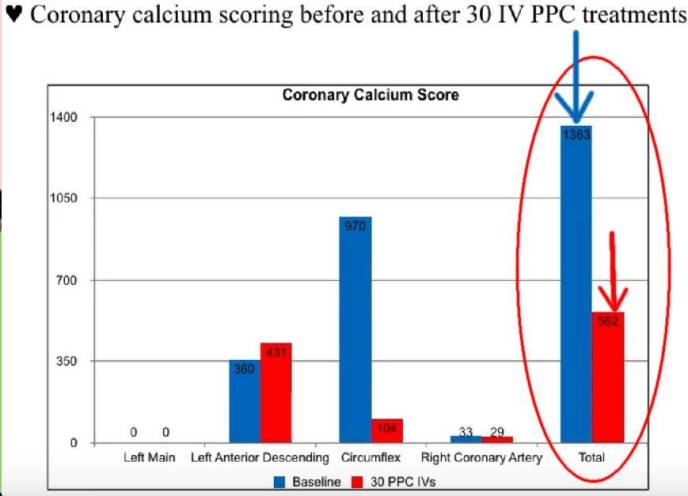
Before treatment Total Calcium Score = 1380 (blue arrow). After 30 IV treatments with essential phospholipid, calcium score reduced to 562 (red arrow), 60% reduction !
The beneficial pleotropic effects of statin drugs can be more effectively replicated, without adverse effects of statins, by using combined modalities of diet, lifestyle modifications and supplements used by integrative practitioners. Here is one such list of items. There are others of course.
Vitamin C (Linus Pauling)
Vitamin K2 – MK7
Magnesium
Vitamin D3
Tocotrienol Vit E
Aged Garlic – Allicin
Essential Phospholipid
Botanicals for NFKB
Address Leaky Gut
Eliminate Wheat
Optimize Hormones
Control Blood Sugar
Fibrinolytic Enzymes
Ozone
EDTA
MTHFR ?
Homocysteine?
Lipoprotein(a) ?
Conclusion:
One of the remarkable paradigm shifts in cardiology is the shift away from the cholesterol panel. The calcium score has emerged as a better decision making tool to decide which patients should be treated with statins, and which patients should not. The old method of prescribing a statin drug based on elevated cholesterol level is no longer valid, and has been replaced by Calcium Score.
Another message supported by the Joshua Mitchell study is the statin drug benefit for the higher calcium score patient is entirely due to pleotropic effects (anti-inflammatory and anti-microbial effects), not due to cholesterol lowering.
No doubt this new methodology will improve the NNT (Number Needed to treat) for the statin drug. However, one must consider the adverse effects of long term statin use, and ask if the trade off is worth the reduction in quality of life? We await further research to answer this question.
Articles with related Interest:
Coronary Calcium Score Benefits of Aged Garlic
Diabetes Arterial Calcification and Statin Drugs
All Past Heart Disease Articles by Jeffrey Dach MD
Jeffrey Dach MD
7450 Griffin Road Suite 180
Davie, Fl 33314
954-792-4663
References:
1) Society of Cardiovascular Computed Tomography consensus statement using a CAC threshold of 100 for treatment
2) Mitchell, Joshua D., et al. “Impact of statins on cardiovascular outcomes following coronary artery calcium scoring.” Journal of the American College of Cardiology 72.25 (2018): 3233-3242.
Link to full pdf: Coronary artery calcium death myocardial infarction walter reed Mitchell Joshua JACC Card Imaging 2018.
3) Raggi, Paolo. “Coronary calcium is all we need for risk assessment, yet we do not use it often enough.” Atherosclerosis (2019).
The most fatal flaw of CAC detection for risk assessment, in the eye of physicians opposed to its use, is that there are no randomized clinical trials to demonstrate that by treating only patients with CAC, as opposed to those with an (no ?) indication for treatment, the risk of events is reduced. However, the circumstantial evidence that this is true is overwhelming, and it is simply logical to predict that antibiotics will work best in patients with lobar pneumonia than in those at “risk of developing pneumonia”.
4) Abstract 20067: Impact of Statins on Long-Term Cardiovascular Outcomes in Patients Undergoing Coronary Artery Calcium Scoring: Results From the Walter Reed Registry
Joshua D Mitchell , Nicole Fergestrom , Patrick Moon , Robert Paisley
, and Todd C Villines Originally published 29 Mar 2018 Circulation. 2018;134:A20067
Abstract
Introduction: Coronary artery calcium (CAC) scoring significantly improves cardiovascular risk prediction as compared to standard cardiovascular risk factors. However, the impact of statins on atherosclerotic cardiovascular disease (ASCVD) events among subjects undergoing coronary calcium scoring is not known.
Methods: We identified consecutive subjects without pre-existing ASCVD or malignancy who underwent CAC scoring (Agatston) at Walter Reed Medical Center from 2001-2009. Outcomes, baseline risk factors, and individual prescription data were extracted from the military data repository, a comprehensive healthcare database that captures care provided within and outside of the military healthcare system. Patient-level death data were acquired from the National Death Index. Subjects were assessed for the primary outcome of first major adverse cardiac event (MACE), a composite of myocardial infarction, stroke and cardiovascular death. Outcomes were analyzed using Cox proportional hazard multivariate regression controlling for baseline ASCVD risk factors and using a time dependent variable to account for statin exposure.
Results: 14,956 patients (mean age 50 years; 71 % men) were followed for a mean of 9.3 ± 2.8 years. Among all patients, statin therapy was an independent predictor for reduced MACE (adjusted hazard ratio 0.79, 95% CI 0.66-0.94). Comparing statin treated patients to those not treated with statins, the number needed to treat (NNT) for 1 year to prevent one incident MACE outcome ranged from 3950.9 patients (CAC=0) to 45.3 patients (CAC >400) (Table 1).
Conclusion: In a large-scale cohort without baseline ASCVD, CAC presence and severity significantly risk stratified patients who are most and least likely to benefit from statin therapy during long-term follow-up.
5) Curtis, Michael, et al. “Effect of Dose and Timing of Preoperative Statins on Mortality After Coronary Artery Bypass Surgery.” The Annals of Thoracic Surgery (2017).
6) Barakat, Amr F., et al. “Perioperative statin therapy for patients undergoing coronary artery bypass grafting.” The Annals of thoracic surgery 101.2 (2016): 818-825.
7) Hennessy, Emma, et al. “Is there potential for repurposing statins as novel antimicrobials?.” Antimicrobial agents and chemotherapy 60.9 (2016): 5111-5121.
8) Patel, Tushar R., and Siobhan A. Corbett. “Simvastatin suppresses LPS-induced Akt phosphorylation in the human monocyte cell line THP-1.” Journal of Surgical Research 116.1 (2004): 116-120.
9) Devaraj et al “Direct demonstration of an antiinflammatory effect of simvastatin in subjects with the metabolic syndrome.” J Clin Endo & Metab 91.11 (2006): 4489-4496.
10) Hölschermann, Hans, et al. “Statins prevent NF-κB transactivation independently of the IKK-pathway in human endothelial cells.” Atherosclerosis 185.2 (2006): 240-245.
11) Lincoff, A. Michael, et al. “Evacetrapib and cardiovascular outcomes in high-risk vascular disease.” New Eng J Medicine 376.20 (2017): 1933–1942.
12) Chukkapalli, Sasanka S., et al. “Polymicrobial oral infection with four periodontal bacteria orchestrates a distinct inflammatory response and atherosclerosis in ApoEnull mice.” PLoS One 10.11 (2015): e0143291.
13) Chukkapalli, Sasanka S., et al. “Sequential colonization of periodontal pathogens in induction of periodontal disease and atherosclerosis in LDLRnull mice.” Pathogens and disease 75.1 (2017).
14) Chhibber-Goel, Jyoti, et al. “Linkages between oral commensal bacteria and atherosclerotic plaques in coronary artery disease patients.” NPJ biofilms and microbiomes 2.1 (2016): 7.
15) Dykun, Iryna, et al. “Statin medication enhances progression of coronary artery calcification: the Heinz Nixdorf Recall Study.” Journal of the American College of Cardiology 68.19 (2016): 2123-2125
16) Raggi, Paolo, Tracy Q. Callister, and Leslee J. Shaw. “Progression of coronary artery calcium and risk of first myocardial infarction in patients receiving cholesterol-lowering therapy.” Arteriosclerosis, thrombosis, and vascular biology 24.7 (2004): 1272-1277.
17) Hecht, Harvey S. “Coronary artery calcium scanning: past, present, and future.” JACC: Cardiovascular Imaging 8.5 (2015): 579-596.
Last updated on March 19th, 2019 by
The post Calcium Score Determines Who to Treat With Statin Drug appeared first on Jeffrey Dach MD.









Leave a Comment
You must be logged in to post a comment.