I was intrigued by a 2015 case report by John Rodakis of an autistic child whose symptoms dramatically improved while on a 10 day course of antibiotics.(4) The dad brought the autistic child to an urgent care center, where strep thoat was diagnosed and a 10 day course of Amoxicillin prescribed. On the fourth day of Amoxicillin, the dad noticed the child began making eye contact, which he had previously avoided. The child’s speech began to improve markedly, and his compulsive repetitive behaviors decreased etc. The author speculated that the antibiotics had a favorable effect on the child’s gut flora, also called the microbiome. Left image image of bacteria courtesy of MMRF.
Gut Dysbioisis in Autism
This is not an isolated observation. Fifteen years earlier, Dr Finegold reported in the Journal of Child Neurology short term improvement in autistic children with the antibiotic, Vancomycin.(5) Dr. Finegold speculated in some autistic children, exposure to antibiotics causes “disruption of indigenous gut flora promoting colonization by neurotoxin-producing bacteria,” The author ran a trial study with 11 autistic children treated with the oral antibiotic vancomycin. Short term improvement was documented. Unfortunately the improvements were temporary and waned on later follow up. The author speculated that this small study indicated a possible gut flora-brain connection in autism. Left image vancomycin courtesy of Hospira.
Leaky Gut and Dysbiosis in a Mouse Model of Autism
Dr Elaine Y. Hsiao et al, in a 2013 report in Cell stated that many autistic children “display dysbiosis of the gut microbiota, and some exhibit increased intestinal permeability. “(6) The authors noted three studies reporting significantly elevated levels of the pathogenic bacteria, Clostridium in Autism (Finegold et al., 2002; Parracho et al., 2005; Song et al., 2004). Left image autism mouse model courtesy of Psy Post.
Dr Elaine Y. Hsiao et al. studied a mouse model of autism in which the maternal mice were injected with the viral mimic, polyinosinic: polycytidylic acid (poly I:C), a synthetic analog of double-stranded RNA. serving as an immune system stimulant which induces fever and inflammation. The offspring of such maternal mice treated with Poly I:C exhibit autistic behaviors, and the same “leaky gut” ie. increased intestinal permeability, and disruption of gut flora (ie dysbiosis) similar to autistic human children.. In this mouse model of autism, treatment with a probiotic, Bacteroides Fragilis, restored gut integrity and rebalanced the gut microbiota, to normal. Probiotic treatment also ameliorated autism symptoms with improved communicative, repetitive, and anxiety-like behavior in the autistic mice, a finding supporting a “gut-brain link” in Autism Spectrum Disorder.
Gut Flora in Autism Differs From Normal Children
In a 2005 report, Dr. Parracho et al. studied the fecal flora of autistic children, finding “The faecal flora of ASD patients contained a higher incidence of the Clostridium histolyticum group (Clostridium clusters I and II) of bacteria than that of healthy children”. (7) The authors also noted that ” Clostridia organisms are toxin-producers and their metabolic products also exerting systemic effects. ” Left image Clostridium courtesy of Micro Be WIld.
Clostridia Metabolites and Autism – Propionic Acid
One of the toxic metabolites of Clostridia in the gut is propionic acid. Dr McFabe wrote a review in 2013 on the role propionic acid, in autism. In mouse models, studies show that “propionic acid-treated rats display Autism-like repetitive, perseverative, and antisocial behaviors and seizure. Neurochemical changes, consistent and predictive with findings in Autism Spectrum Disorder (ASD) patients, including neuroinflammation, increased oxidative stress, mitochondrial dysfunction, glutathione depletion have been observed.”
Another Clostrida metobolite is P-Cresol
Massive quantities of metabolites, P-cresol and HPHPA (propionic acid) are produced by the overgown clostridia in the disturbed gut of autistic children. (13). These two metabolites inhibit the enzyme Dopamine Beta Hydroxylase, responsible for converting Dopamine to norepinephrine and epinephiene. This inhibition of Dopamine Beta Hydroxylase results in a build up of excess dopamine, and a deficiency in norepinephrine.(13) Under such conditions, the dopamine metabolite HVA (homo-vanillic acid) is increased in large quantities in urine samples of autistic children. According to Dr William Shaw, excess dopamine is pathogenic, producing obsessive compulsive behavior and free radical damage in the brain worsened by glutathione depletion. (13)
Drugs That Cause Depletion of Glutathione – Tylenol
Tylenol (acetaminophen) is a drug known to deplete glutathione, and has been implicated in etiology of autism. (14,15) Because of this revelation, the routine use of tylenol for febrile young children after vaccination is no longer recommended. Left image courtesy of Health Impact news.
Clostridia Metabolites Cause Autism and Schizophrenia
In 2010 William Shaw reported high levels of HPHPA (hydroxy-propionic acid) in urine samples of patients with autism and schizophrenia. HPHPA is an abnormal phenylalanine metabolite of Clostridia species, a pathogenic bacteria in the gastrointestinal tract. Dr Saw states:
“The highest value (of HPHPA) measured in urine samples was 300 times the median normal adult value, in a patient with acute schizophrenia during an acute psychotic episode. The psychosis remitted after treatment with oral vancomycin with a concomitant marked decrease in HPHPA. The source of this compound appears to be multiple species of anaerobic bacteria of the Clostridium genus. The significance of this compound is that it is a probable metabolite of m-tyrosine (3-hydroxyphenylalanine), a tyrosine analog which depletes brain catecholamines and causes symptoms of autism (stereotypical behavior, hyperactivity, and hyper-reactivity) in experimental animals.” (16,17)
Testing for Urinary Metabolites can be done using the organic acids test performed by various laboratoiries such as Great Plains Lab, and Genova Lab (previously Metametrix).
A useful book available from Kirkland labs is recommended for further study.(18)
Glyphosate – The Elephant in the Room
The herbicide Roundup which contains glyphosate manufactured by Monsanto has received attention because animal studies show dysbiosis and disruption of gut flora in animals treated with glyphosate. (21-24) A series of animal studies by Dr. Kruger shows that glyphosate acts as an antimicrobial to gut bacteria preferentially killing beneficial bacteria while allowing pathogenic bacteria such as Clostridia and Salmonella to survive.(21-24) Dr Kruger says:
“evidence that the highly pathogenic bacteria as Salmonella Entritidis, Salmonella Gallinarum, Salmonella Typhimurium, Clostridium perfringens and Clostridium botulinum are highly resistant to glyphosate. However, most of beneficial bacteria as Enterococcus faecalis, Enterococcus faecium, Bacillus badius, Bifidobacterium adolescentis and Lactobacillus spp. were found to be moderate to highly susceptible. … A reduction of beneficial bacteria in the gastrointestinal tract microbiota by ingestion of glyphosate could disturb the normal gut bacterial community. “
Above left image courtesy of Dr Stephanie Seneff MIT Power Point Presentation: SeneffGlyphosateYale2014-2-Elephant in the Room
The Shikimate Pathway
Glyphosate was deemed safe for humans because it blocks an enzyme system in plants called the Shikimate pathway, a biochemical pathway which does not exist in humans. However, regulators forgot to consider the effect of glyphosate on friendly gut bacteria which do use the Shikimate pathway . The friendly gut bacteria are killed, and the pathogenic bacteria resistant to glyphosate survive. This produces gut dysbiosis similar to that found in autistic children. Which pathogenic bacteria are we left with? You guessed it, the Clostridia. Is it starting to make sense now?
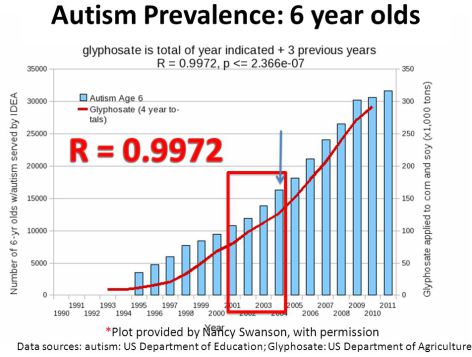
Above chart courtesy of Nancy Swanson showing high correlation between rising autism and glyphosate usage taken from: Genetically engineered crops glyphosate deterioration health United States Swanson J Organic Systems 2014
Holland has just taken steps to ban Glyphosate sale to private individuals. Canada, Brazil, Sri Lanka and the Netherlands have or will soon impose restrictions or bans on glyphosate, the main ingredient in Monsanto’s Roundup weed killer. Now we know why. Glyphosate poses an enormous health risk to human as well as plant life.
Articles with Related Interest: Dr Oz Smear Campaign Backfires.
Jeffrey Dach MD
7450 Griffin Road, Suite 190
Davie, Fl 33314
954 792-4663
Links and References
1) http://press.endocrine.org/doi/full/10.1210/me.2014-1108
Minireview: Gut Microbiota: The Neglected Endocrine Organ
Gerard Clarke,Roman M. Stilling,Paul J. Kennedy,Catherine Stanton,
John F. Cryan, and Timothy G. Dinan Molecular Endocrinology 2014 28:8, 1221-1238
Thus, considering the ability to influence the function of distal organs and systems, in many respects, the gut microbiota resembles an endocrine organ
2) Full pdf: Leaky Gut Autoimmune Diseases Allesio Fasano Clin Review Allergy Immunology 2011
3) Full pdf: Gluten sensitivity from gut to brain Marios Hadjivassiliou Lancet 2010
Autism Responds Dramatically to Antibiotics
Free full text
4) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4374086/
Microb Ecol Health Dis. 2015; 26: 10.3402/mehd.v26.26382.
An n=1 case report of a child with autism improving on antibiotics and a father’s quest to understand what it may mean. John Rodakis*
The author, a parent of a child with autism, describes an n=1 case in which his child’s autism symptoms dramatically and rapidly improved following administration of a common antibiotic. The author asserts that this finding is not unusual in the autism population and that, when combined with prior recent medical research, suggests that a link between autism and the microbiome in some children is not just plausible, but in fact likely for some meaningful percentage of cases. The author argues for increased funding for a more thorough examination of links between autism and the microbiome and poses a series of questions to be further examined in future research. Keywords: autism, microbiome, antibiotic, n=1, N of One, vancomycin, amoxicillin
Thanksgiving Day in the United States is usually a quiet time with family, unless both of your young children contract strep throat while visiting family as ours did in 2012. Because it was a holiday, my wife and I took them to an extended-hours clinic, where a physician confirmed strep via a rapid strep test and prescribed a 10-day course of amoxicillin, one of the most commonly prescribed antibiotics in the United States. Neither had received an antibiotic before and in 2 days they seemed back to normal. This would not be a very interesting story except for what happened next.
Earlier that year our son had been diagnosed with moderate-to-severe autism by a team of clinicians and practitioners at Children’s Medical Center in Dallas, Texas. On day four of his 10-day course of amoxicillin, we began noticing changes in his autism symptoms: he began making eye contact, which he had previously avoided; his speech, which was severely delayed, began to improve markedly; he became less ‘rigid’ in his insistence for sameness and routine; and he also displayed an uncharacteristic level of energy, which he had historically lacked. The improvements continued each day. On day six he rode a tricycle around the room for the first time, alone and unprompted, which was remarkable because we had purchased the tricycle 6 months earlier and had worked with him continuously so he could learn to ride it, however until that point, he had never so much as been able to push the pedals enough to move forward.
5) http://www.ncbi.nlm.nih.gov/pubmed/10921511
J Child Neurol. 2000 Jul;15(7):429-35.
Short-term benefit from oral vancomycin treatment of regressive-onset autism. Sandler RH1, Finegold SM, Bolte ER, Buchanan CP, Maxwell AP, Väisänen ML, Nelson MN, Wexler HM.
Many parents of children with “regressive”-onset autism have noted antecedent antibiotic exposure followed by chronic diarrhea. We speculated that, in a subgroup of children, disruption of indigenous gut flora might promote colonization by one or more neurotoxin-producing bacteria, contributing, at least in part, to their autistic symptomatology. To help test this hypothesis, 11 children with regressive-onset autism were recruited for an intervention trial using a minimally absorbed oral antibiotic. Entry criteria included antecedent broad-spectrum antimicrobial exposure followed by chronic persistent diarrhea, deterioration of previously acquired skills, and then autistic features. Short-term improvement was noted using multiple pre- and post-therapy evaluations. These included coded, paired videotapes scored by a clinical psychologist blinded to treatment status; these noted improvement in 8 of 10 children studied. Unfortunately, these gains had largely waned at follow-up. Although the protocol used is not suggested as useful therapy, these results indicate that a possible gut flora-brain connection warrants further investigation, as it might lead to greater pathophysiologic insight and meaningful prevention or treatment in a subset of children with autism.
Mouse Model of Autism Corrected with Probiotics
6) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3897394/
Cell. 2013 Dec 19; 155(7): 1451–1463.
The microbiota modulates gut physiology and behavioral abnormalities associated with autism . Elaine Y. Hsiao,1,2,* Sara W. McBride,1 Sophia Hsien,1 Gil Sharon,1 Embriette R. Hyde,3 Tyler McCue,3 Julian A. Codelli,2 Janet Chow,1 Sarah E. Reisman,2 Joseph F. Petrosino,3 Paul H. Patterson,1,*† and Sarkis K. Mazmanian1,*†
Although autism spectrum disorder (ASD) is defined by core behavioral impairments, gastrointestinal (GI) symptoms are commonly reported. Subsets of ASD individuals display dysbiosis of the gut microbiota, and some exhibit increased intestinal permeability. Here we demonstrate GI barrier defects and microbiota alterations in a mouse model displaying features of ASD, maternal immune activation (MIA). Oral treatment of MIA offspring with the human commensal Bacteroides fragilis corrects gut permeability, alters microbial composition and ameliorates ASD-related defects in communicative, stereotypic, anxiety-like and sensorimotor behaviors. MIA offspring display an altered serum metabolomic profile, and B. fragilis modulates levels of several metabolites. Treating naïve mice with a metabolite that is increased by MIA and restored by B. fragilis causes behavioral abnormalities, suggesting that gut bacterial effects on the host metabolome impact behavior. Taken together, these findings support a gut-microbiome-brain connection in ASD and identify a potential probiotic therapy for GI and behavioral symptoms of autism.
Autistic Kids have more fecal Clostridium histolyticum than controls.
7) http://www.ncbi.nlm.nih.gov/pubmed/16157555
J Med Microbiol. 2005 Oct;54(Pt 10):987-91.
Differences between the gut microflora of children with autistic spectrum disorders and that of healthy children. Parracho HM1, Bingham MO, Gibson GR, McCartney AL.
Children with autistic spectrum disorders (ASDs) tend to suffer from severe gastrointestinal problems. Such symptoms may be due to a disruption of the indigenous gut flora promoting the overgrowth of potentially pathogenic micro-organisms. The faecal flora of patients with ASDs was studied and compared with those of two control groups (healthy siblings and unrelated healthy children). Faecal bacterial populations were assessed through the use of a culture-independent technique, fluorescence in situ hybridization, using oligonucleotide probes targeting predominant components of the gut flora. The faecal flora of ASD patients contained a higher incidence of the Clostridium histolyticum group (Clostridium clusters I and II) of bacteria than that of healthy children. However, the non-autistic sibling group had an intermediate level of the C. histolyticum group, which was not significantly different from either of the other subject groups. Members of the C. histolyticum group are recognized toxin-producers and may contribute towards gut dysfunction, with their metabolic products also exerting systemic effects. Strategies to reduce clostridial population levels harboured by ASD patients or to improve their gut microflora profile through dietary modulation may help to alleviate gut disorders common in such patients.
Propionic Acid in Autism – MacFabe
8) http://www.ncbi.nlm.nih.gov/pubmed/24416709
Glob Adv Health Med. 2013 Nov;2(6):52-66. doi: 10.7453/gahmj.2013.089.
Autism: metabolism, mitochondria, and the microbiome. Macfabe D1.
New approaches are needed to examine the diverse symptoms and comorbidities of the growing family of neurodevelopmental disorders known as autism spectrum disorder (ASD). ASD originally was thought to be a static, inheritable neurodevelopmental disorder, and our understanding of it is undergoing a major shift. It is emerging as a dynamic system of metabolic and immune anomalies involving many organ systems, including the brain, and environmental exposure. The initial detailed observation and inquiry of patients with ASD and related conditions and the histories of their caregivers and families have been invaluable. How gastrointestinal (GI) factors are related to ASD is not yet clear. Nevertheless, many patients with ASD have a history of previous antibiotic exposure or hospitalization, GI symptoms, abnormal food cravings, and unique intestinal bacterial populations, which have been proposed to relate to variable symptom severity. In addition to traditional scientific inquiry, detailed clinical observation and recording of exacerbations, remissions, and comorbidities are needed. This article reviews the role that enteric short-chain fatty acids, particularly propionic (also called propanoic) acid, produced from ASD-associated GI bacteria, may play in the etiology of some forms of ASD. Human populations that are partial metabolizers of propionic acid are more common than previously thought. The results from pre-clinical laboratory studies show that propionic acid-treated rats display ASD-like repetitive, perseverative, and antisocial behaviors and seizure. Neurochemical changes, consistent and predictive with findings in ASD patients, including neuroinflammation, increased oxidative stress, mitochondrial dysfunction, glutathione depletion, and altered phospholipid/acylcarnitine profiles, have been observed.
Propionic acid has bioactive effects on (1) neurotransmitter systems, (2) intracellular acidification and calcium release, (3) fatty acid metabolism, (4) gap junction gating, (5) immune function, and (6) alteration of gene expression that warrant further exploration. Traditional scientific experimentation is needed to verify the hypothesis that enteric short-chain fatty acids may be a potential environmental trigger in some forms of ASD. Novel collaborative developments in systems biology, particularly examining the role of the microbiome and its effects on host metabolism, immune and mitochondrial function, and gene expression, hold great promise in ASD.
9) Al-Owain, M., et al. “Autism spectrum disorder in a child with propionic acidemia.” JIMD Reports-Case and Research Reports, 2012/4. Springer Berlin Heidelberg, 2013. 63-66.
10) https://www.autismspeaks.org/science/science-news/spotlight-gut-bacteria-brain-connection-autism
Researchers explore how disruptions in the intestine’s community of digestive bacteria may influence brain development and autism
November 13, 2013
11) http://cogentbenger.com/autism/interviews/macfabe-interview/
Dr. Derrick MacFabe Interview
Patent William Shaw on Urine Organic Acid Testing in Autism
12) http://www.google.com/patents/US5686311
Diagnosis of autism and treatment therefor
A method for diagnosing the likelihood of autism in patients is provided which comprises first obtaining from the patient a sample of body fluid such as urine and analyzing the sample to determine the quantity therein of at least one marker compound selected from the group consisting of citramalic acid, 5-hydroxy-methyl-2-furoic acid, 3-oxo-glutaric acid, furan-2,5-dicarboxylic acid, tartaric acid, furancarbonylglycine, arabinose, dihydroxyphenylpropionic acid, carboxycitric acid and phenylcarboxylic acid; if the quantities of one or more of the compounds are abnormally high, as compared with the urine of non-autistic individuals, an ultimate diagnosis of autism is likely. The invention also pertains to a method of treating autistic patients by administration of antifungal drugs, in order to ameliorate the clinical symptoms of autism.
Inventors William Shaw
13) Inhibition of dopamine conversion to norepinephrine by Clostridia 2012 William Shaw
P cresol and HPHPA are produced in massive quantities by the overgown clostridia. These inhibit Dopamne Beta Hydroxylase.with over production of fopamine and underproduction of norepinephrine. Major fopamine metabolite HVA is increased in urine.
Obsessive compulsive stereotypical behavior is associated with Dopamine excess.
Excess dopamine causes free radical damage worsened by glutathione depletion.
14) Tylenol_Acetaminophen_Glutathione__Autism_William Shaw_2013
15) Acetaminophen (Tylenol) and the autism epidemic November 10, 2014 Dr. Manuel Casanova made his residency training in neurology and then spent 3 years doing a fellowship in neuropathology at The Johns Hopkins Hospital. During his stay at the Johns Hopkins Hospital, Dr. Casanova was in-charge of Pediatric Neuropathology
Proprionic Acid HHPA – William Shaw
16) Increased Propionic acid HPHPA Clostridia in Autism Willima Shaw_2010 full pdf file
17) http://www.ncbi.nlm.nih.gov/pubmed/20423563
Nutr Neurosci. 2010 Jun;13(3):135-43. Increased urinary excretion of a 3-(3-hydroxyphenyl)-3-hydroxypropionic acid (HPHPA), an abnormal phenylalanine metabolite of Clostridia spp. in the gastrointestinal tract, in urine samples from patients with autism and schizophrenia. by William Shaw
A compound identified as 3-(3-hydroxyphenyl)-3-hydroxypropionic acid (HPHPA) was found in higher concentrations in urine samples of children with autism compared to age and sex appropriate controls and in an adult with recurrent diarrhea due to Clostridium difficile infections. The highest value measured in urine samples was 7500 mmol/mol creatinine, a value 300 times the median normal adult value, in a patient with acute schizophrenia during an acute psychotic episode. The psychosis remitted after treatment with oral vancomycin with a concomitant marked decrease in HPHPA. The source of this compound appears to be multiple species of anaerobic bacteria of the Clostridium genus. The significance of this compound is that it is a probable metabolite of m-tyrosine (3-hydroxyphenylalanine), a tyrosine analog which depletes brain catecholamines and causes symptoms of autism (stereotypical behavior, hyperactivity, and hyper-reactivity) in experimental animals.
18) KIRKMAN_BOOK_Guide_Intestinal_Health_Autism_Gut_Brain
A comprehensive review of intestinal health issues in Autism Spectrum Disorders and the options available for treating them. Authored By Kirkman Labs’ Technical Staff: Mark Brudnak, N. D., Ph. D. Ilene Buchholz, R. N. Stephanie Hoener, N. D. Larry Newman, Chemist Jon Pangborn, Ph. D.,
19) Severe Neurological and Psychiatric Disorders Caused by
Gastrointestinal Overgrowth of Clostridia Bacteria. Mechanism and
Treatment; A lecture by William Shaw PhD at ICIM Nashville March
14 16, 2014
Although dysbiosis or abnormal microbial overgrowth of the gastrointestinal
tract has long been suspected of causing psychiatric disorders, the exact
mechanism was unknown. For the first time, William Shaw Ph.D. presents
convincing evidence that certain Clostridia bacteria produce phenolic metabolites that dramatically alter the conversion of dopamine to norepinephrine, leading to profound dopamine excess and severe depletion of norepinephrine and epinephrine in the brain, peripheral sympathetic nervous system and adrenal glands. Furthermore, the excess dopamine leads to oxidative stress that can result in permanent damage to the brain, sympathetic nervous system, and adrenal glands if not treated. He will present a variety of case studies of patients with autism, depression,
schizophrenia, and other neuropsychiatric disorders showing the usefulness of urine organic acid testing in the diagnosis and treatment of these disorders.
20) Buy on Amazon: William Shaw Book Biological Treatments for Autism and PDD
————————————————–
glyphosate
21) http://www.ncbi.nlm.nih.gov/pubmed/23224412
Curr Microbiol. 2013 Apr;66(4):350-8. doi: 10.1007/s00284-012-0277-2. Epub 2012 Dec 9. The effect of glyphosate on potential pathogens and beneficial members of poultry microbiota in vitro. Shehata AA1, Schrödl W, Aldin AA, Hafez HM, Krüger M.
The use of glyphosate modifies the environment which stresses the living microorganisms. The aim of the present study was to determine the real impact of glyphosate on potential pathogens and beneficial members of poultry microbiota in vitro.
The presented results evidence that the highly pathogenic bacteria as Salmonella Entritidis, Salmonella Gallinarum, Salmonella Typhimurium, Clostridium perfringens and Clostridium botulinum are highly resistant to glyphosate. However, most of beneficial bacteria as Enterococcus faecalis, Enterococcus faecium, Bacillus badius, Bifidobacterium adolescentis and Lactobacillus spp. were found to be moderate to highly susceptible. Also Campylobacter spp. were found to be susceptible to glyphosate. A reduction of beneficial bacteria in the gastrointestinal tract microbiota by ingestion of glyphosate could disturb the normal gut bacterial community. Also, the toxicity of glyphosate to the most prevalent Enterococcus spp. could be a significant predisposing factor that is associated with the increase in C. botulinum-mediated diseases by suppressing the antagonistic effect of these bacteria on clostridia.
Glyphosate linked to botulism and other animal health problems
Three very interesting papers from Monika Kruger and her team in Leipzig on the effect glyphosate has on the gut micro-organisma in animals by damaging the beneficial bacteria
“A reduction of beneficial bacteria in the gastrointestinal tract microbiota by ingestion of glyphosate could disturb the normal gut bacterial community.”
There is now a strong probability that glyphosate residues in animal feeds result in botulism in the cattle and also in related ailments in poultry.
22) Visceral botulism at dairy farms in Schleswig Holstein, Germany – Prevalence of Clostridium botulinum in feces of cows, in animal feeds, in feces of the farmers, and in house dust by Monika Krüger, Anke Große-Herrenthey, Wieland Schrödl, Achim Gerlach, Arne Rodloff Anaerobe 18 (2012) 221e223 Accepted 11 December 2011 Available online 21 December 2011
From 41 dairy farms in Schleswig Holstein, Germany, 196 fecal specimens of diseased cows, 77 fecal specimens of farmers and family members from 26 of these farms, 35 animal feed specimens and 7 house dust specimens were investigated for Clostridium botulinum and its antigens, respectively. Four of the humans under study (one child, 8 month, and three adults) showed symptoms of infant/visceral botulism. Specimens were cultivated in reinforced clostridial medium (RCM). C. botulinum antigens were detected by ELISA. The aim of the study was to obtain information on the relationship of detected C. botulinum toxin-types in cows, in the feces of attending humans, and in the immediate environment. The results revealed that C. botulinum toxin-types were different for cows and humans. Toxin-type A was dominant in cow feces while type E was found in humans. Type E was also present in some animal feed specimens. Conversely, toxin-type A was prevalent in the house dust of farms. It may be assumed that the feeds were the source of human colonization with C. botulinum.
23) Effect Glyphosate Pathogens Poultry Microbiota In Vitro Krueger Shehata Curr Microbiol 2012
The Effect of Glyphosate on Potential Pathogens and Beneficial Members of Poultry Microbiota In Vitro by Awad A. Shehata, Wieland Schro¨dl, Alaa. A. Aldin, Hafez M. Hafez , and Monika Kru¨ger Curr Microbiol 2012 Springer
The use of glyphosate modifies the environment which stresses the living microorganisms. The aim of the present study was to determine the real impact of glyphosate on potential pathogens and beneficial members of poultry microbiota in vitro. The presented results evidence that the highly pathogenic bacteria as Salmonella Entritidis, Salmonella Gallinarum, Salmonella Typhimurium, Clostridium perfringens and Clostridium botulinum are highly resistant to glyphosate. However, most of beneficial bacteria as Enterococcus faecalis, Enterococcus faecium, Bacillus badius, Bifidobacterium adolescentis and Lactobacillus spp. were found to be moderate to highly susceptible. Also Campylobacter spp. were found to be susceptible to glyphosate. A reduction of beneficial bacteria in the gastrointestinal tract microbiota by ingestion of glyphosate could disturb the normal gut bacterial community. Also, the toxicity of glyphosate to the most prevalent Enterococcus spp. could be a significant predisposing factor that is associated with the increase in C. botulinum-mediated diseases by suppressing the antagonistic effect of these bacteria on clostridia.
24) Glyphosate suppresses the antagonistic effect of Enterococcus on Clostridia Kruger 2013 by Monika Krüger, Awad Ali Shehata, Wieland Schrödl, Arne Rodloff. Anaerobe 20 (2013) 74e78
During the last 15 years, an increase of Clostridium botulinum associated diseases in cattle has been observed in Germany. The reason for this development is currently unknown. The normal intestinal microflora is a critical factor in preventing intestinal colonisation by C. botulinum as shown in the mouse model of infant botulism. Numerous bacteria in the gastro-intestinal tract (GIT) produce bacteriocines directed against C. botulinum and other pathogens: Lactic acid producing bacteria (LAB) such as lactobacilli, lactococci and enterococci, generate bacteriocines that are effective against Clostridium spp. A reduction of LAB in the GIT microbiota by ingestion of strong biocides like glyphosate could be an explanation for the observed increase in levels of C. botulinum associated diseases. In the present paper, we report on the toxicity of glyphosate to the most prevalent Enterococcus spp. in the GIT. Ingestion of this herbicide could be a significant predisposing factor that is associated with the increase in C. botulinum mediated diseases in cattle.
25) http://healthimpactnews.com/2014/the-microbiota-crisis-how-the-herbicide-glyphosate-is-killing-microbiomes/
by Martin Michener, PhD Health Impact News Healthy Gut Flora: Key to Health
P-Cresol in Autism Children
26) http://www.ncbi.nlm.nih.gov/pubmed/25010144
Biomarkers. 2014 Sep;19(6):463-70. doi: 10.3109/1354750X.2014.936911. Epub 2014 Jul 10.
Urinary p-cresol is elevated in young French children with autism spectrum disorder: a replication study. Gabriele S1, Sacco R, Cerullo S, Neri C, Urbani A, Tripi G, Malvy J, Barthelemy C, Bonnet-Brihault F, Persico AM.
The aromatic compound p-cresol (4-methylphenol) has been found elevated in the urines of Italian autistic children up to 8 years of age. The present study aims at replicating these initial findings in an ethnically distinct sample and at extending them by measuring also the three components of urinary p-cresol, namely p-cresylsulfate, p-cresylglucuronate and free p-cresol. Total urinary p-cresol, p-cresylsulfate and p-cresylglucuronate were significantly elevated in 33 French autism spectrum disorder (ASD) cases compared with 33 sex- and age-matched controls (p < 0.05). This increase was limited to ASD children aged ≤8 years (p < 0.01), and not older (p = 0.17). Urinary levels of p-cresol and p-cresylsulfate were associated with stereotypic, compulsive/repetitive behaviors (p < 0.05), although not with overall autism severity. These results confirm the elevation of urinary p-cresol in a sizable set of small autistic children and spur interest into biomarker roles for p-cresol and p-cresylsulfate in autism.
Amino Acid Profile in Autistic Children – Lower levels of Tryptophan and Phenyl-Alanine in Autistic children
27) Autistic children exhibit distinct plasma amino acid profile Shaik Mohammad Naushad 2013
Indian Journal of Biochemistry & Biophysics Vol. 50, October 2013, pp. 474-478 Short Communication Autistic children exhibit distinct plasma
amino acid profile Shaik Mohammad Naushad
In order to ascertain whether autistic children display characteristic metabolic signatures that are of diagnostic value, plasma amino acid analyses were carried out on a cohort of 138 autistic children and 138 normal controls using reverse-phase HPLC. Pre-column derivatization of amino acids with phenyl isothiocyanate forms phenyl thio-carbamate derivates that have a lamba(max) of 254 nm, enabling their detection using photodiode array. Autistic children showed elevated levels of glutamic acid (120 +/- 89 vs. 83 +/- 35 micromol/L) and asparagine (85 +/- 37 vs. 47 +/- 19 micromol/L); lower levels of phenylalanine (45 +/- 20 vs. 59 +/- 18 micromol/L), tryptophan (24 +/- 11 vs. 41 +/- 16 micromol/L), methionine (22 +/- 9 vs. 28 +/- 9 micromol/L) and histidine (45 +/- 21 vs. 58 +/- 15 micromol/L). A low molar ratio of (tryptophan/large neutral amino acids) x 100 was observed in autism (5.4 vs 9.2), indicating lesser availability of tryptophan for neurotransmitter serotonin synthesis. To conclude, elevated levels of excitatory amino acids (glutamate and asparagine), decreased essential amino acids (phenylalanine, tryptophan and methionine) and decreased precursors of neurotransmitters (tyrosine and tryptophan) are the distinct characteristics of plasma amino acid profile of autistic children. Thus, such metabolic signatures might be useful tools for early diagnosis of autism.
——————————————
A Book Exposing Fraud at the FDA, Subversion of Science…Lies etc.
28) Altered Genes, Twisted Truth: How the Venture to Genetically Engineer Our Food Has Subverted Science, Corrupted Government, and Systematically Deceived the Public by Steven Druker
This book uncovers the biggest scientific fraud of our age. It tells the fascinating and frequently astounding story of how the massive enterprise to restructure the genetic core of the world’s food supply came into being, how it advanced by consistently violating the protocols of science, and how for more than three decades, hundreds of eminent biologists and esteemed institutions have systematically contorted the truth in order to conceal the unique risks of its products—and get them onto our dinner plates.
Altered Genes, Twisted Truth gives a graphic account of how this elaborate fraud was crafted and how it not only deceived the general public, but Bill Clinton, Bill Gates, Barack Obama and a host of other astute and influential individuals as well. The book also exposes how the U.S. Food and Drug Administration (FDA) was induced to become a key accomplice—and how it has broken the law and repeatedly lied in order to usher genetically engineered foods onto the market without the safety testing that’s required by federal statute. As a result, for fifteen years America’s families have been regularly ingesting a group of novel products that the FDA’s own scientific staff had previously determined to be unduly hazardous to human health.
By the time this gripping story comes to a close, it will be clear that the degradation of science it documents has not only been unsavory but unprecedented—and that in no other instance have so many scientists so seriously subverted the standards they were trained to uphold, misled so many people, and imposed such magnitude of risk on both human health and the health of the environment.
29) Glyphosate Roundup Human Placental Cells Aromatase Seralini Richard 2005 Env Health Persp Richard, Sophie, et al. “Differential effects of glyphosate and roundup on human placental cells and aromatase.” Environmental health perspectives (2005): 716-720.
30) pdf Glyphosate-based herbicides are toxic and endocrine disruptors in human cell lines_Seralini_Gasnier_Toxicology_2009
Gasnier, Céline, et al. “Glyphosate-based herbicides are toxic and endocrine disruptors in human cell lines.” Toxicology 262.3 (2009): 184-191.
Autism and the Microbiome MACFABE
31) http://www.ncbi.nlm.nih.gov/pubmed/24416709
Glob Adv Health Med. 2013 Nov;2(6):52-66.
Autism: metabolism, mitochondria, and the microbiome.
Macfabe D1. 1The Kilee Patchell-Evans Autism Research Group, Departments of Psychology (Neuroscience) and Psychiatry, Division of Developmental Disabilities, Lawson Research Institute, University of Western Ontario, London, Ontario, Canada.
New approaches are needed to examine the diverse symptoms and comorbidities of the growing family of neurodevelopmental disorders known as autism spectrum disorder (ASD). ASD originally was thought to be a static, inheritable neurodevelopmental disorder, and our understanding of it is undergoing a major shift. It is emerging as a dynamic system of metabolic and immune anomalies involving many organ systems, including the brain, and environmental exposure. The initial detailed observation and inquiry of patients with ASD and related conditions and the histories of their caregivers and families have been invaluable. How gastrointestinal (GI) factors are related to ASD is not yet clear. Nevertheless, many patients with ASD have a history of previous antibiotic exposure or hospitalization, GI symptoms, abnormal food cravings, and unique intestinal bacterial populations, which have been proposed to relate to variable symptom severity. In addition to traditional scientific inquiry, detailed clinical observation and recording of exacerbations, remissions, and comorbidities are needed. This article reviews the role that enteric short-chain fatty acids, particularly propionic (also called propanoic) acid, produced from ASD-associated GI bacteria, may play in the etiology of some forms of ASD. Human populations that are partial metabolizers of propionic acid are more common than previously thought. The results from pre-clinical laboratory studies show that propionic acid-treated rats display ASD-like repetitive, perseverative, and antisocial behaviors and seizure. Neurochemical changes, consistent and predictive with findings in ASD patients, including neuroinflammation, increased oxidative stress, mitochondrial dysfunction, glutathione depletion, and altered phospholipid/acylcarnitine profiles, have been observed. Propionic acid has bioactive effects on (1) neurotransmitter systems, (2) intracellular acidification and calcium release, (3) fatty acid metabolism, (4) gap junction gating, (5) immune function, and (6) alteration of gene expression that warrant further exploration. Traditional scientific experimentation is needed to verify the hypothesis that enteric short-chain fatty acids may be a potential environmental trigger in some forms of ASD. Novel collaborative developments in systems biology, particularly examining the role of the microbiome and its effects on host metabolism, immune and mitochondrial function, and gene expression, hold great promise in ASD.
Autism spectrum disorder; animal model; carnitine; clostridia; fatty acids; gap junctions; gastrointestinal tract; microbiome; mitochondria; neuropsychiatric disorder; propanoic acid; propionic acid
Free PMC Article
32) MacFabe, Derrick F. “Short-chain fatty acid fermentation products of the gut microbiome: implications in autism spectrum disorders.” Microbial ecology in health and disease 23 (2012).
33) Genetically engineered crops glyphosate deterioration health United States_Nov_2014_Swanson. Swanson, Nancy L., et al. “Genetically engineered crops, glyphosate and the deterioration of health in the United States of America.” Journal of Organic Systems 9.2 (2014): 6-37.
34) Roundup Glyphosate Converging Pattern of Toxicity Farm to Clinic to Laboratory Studies, We need to ban glyphosate from our own communities as most governments fail to protect citizens by Dr Eva Sirinathsinghj ISIS 2015
Power point presentations
35) The Spectrum of Gluten Intolerance Beyond Celiac Disease
www.ibstreatmentcenter.com/Articles/WangenGIG08.ppt
%2020.pdf
37) Unlocking the Secrets of Gluten Sensitivity. Implications for Neurological, Musculoskeletal,and Immune Health. Thomas O’Bryan, D.C. March 2008
38) http://www.slideshare.net/metametrix/the-gutbrain-connection-an-inside-look-at-depression
Published on Jun 24, 2009 During a recent Metametrix sponsored breakfast at the IFM Symposium in Hollywood, Florida, Dr. Todd LePine gave a compelling presentation entitled The Gut-Brain Connection: An Inside Look at Depression.
Kriss Kresser: http://chriskresser.com/the-healthy-skeptic-podcast-episode-9/
http://www.ncbi.nlm.nih.gov/pubmed/21054680
Neurogastroenterol Motil. 2011 Mar;23(3):255-64, e119. doi: 10.1111/j.1365-2982.2010.01620.x. Epub 2010 Nov 5. Reduced anxiety-like behavior and central neurochemical change in germ-free mice. Neufeld KM1, Kang N, Bienenstock J, Foster JA.
There is increasing interest in the gut-brain axis and the role intestinal microbiota may play in communication between these two systems. Acquisition of intestinal microbiota in the immediate postnatal period has a defining impact on the development and function of the gastrointestinal, immune, neuroendocrine and metabolic systems. For example, the presence of gut microbiota regulates the set point for hypothalamic-pituitary-adrenal (HPA) axis activity.
METHODS: We investigated basal behavior of adult germ-free (GF), Swiss Webster female mice in the elevated plus maze (EPM) and compared this to conventionally reared specific pathogen free (SPF) mice. Additionally, we measured brain mRNA expression of genes implicated in anxiety and stress-reactivity.
KEY RESULTS: Germ-free mice, compared to SPF mice, exhibited basal behavior in the EPM that can be interpreted as anxiolytic. Altered GF behavior was accompanied by a decrease in the N-methyl-D-aspartate receptor subunit NR2B mRNA expression in the central amygdala, increased brain-derived neurotrophic factor expression and decreased serotonin receptor 1A (5HT1A) expression in the dentate granule layer of the hippocampus.
CONCLUSIONS & INFERENCES:We conclude that the presence or absence of conventional intestinal microbiota influences the development of behavior, and is accompanied by neurochemical changes in the brain.
Bilbo, Staci D., Cynthia D. Nevison, and William Parker. “A model for the induction of autism in the ecosystem of the human body: the anatomy of a modern pandemic?.” Microbial ecology in health and disease 26 (2015).
The post Curing Autism with Antibiotics appeared first on Jeffrey Dach MD .










jeffrey_dach_md April 8, 2015 at 10:35 AM
Update 4/8/15
The Risk for developing Cancer Depends on Type and location of the BRCA Mutation: Risk of Breast and Ovarian Cancer May Differ By Type of BRCA1, BRCA2 Mutation JAMA APRIL 7, 2015 Timothy R. Rebbeck, Ph.D