Progesterone for PMS, and irregular menstrual cycles. Part Two
For over a million years, now, estrogen and progesterone has been key players in the female menstrual cycle, ovulation and fertility. Left Image: Iconic 1966 theatrical poster of Raquel Welch in One Million Years BC. later featured in the Shawshank Redemption covering the escape tunnel.
Understanding the Normal Menstrual Cycle – Hormone Charts
The chart below from college level biology class, showing the idealized normal menstrual cycle.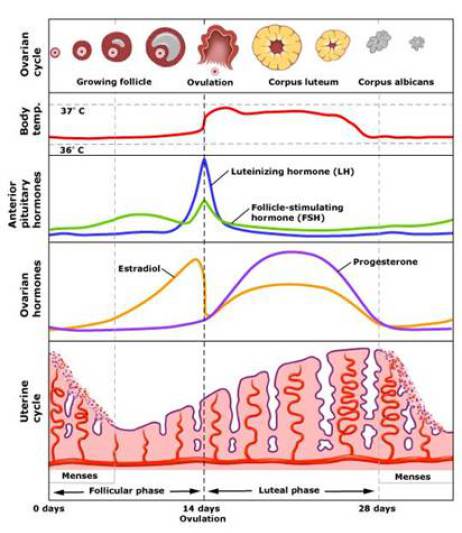 Estrogen and Progesterone
Estrogen and Progesterone
To understand progesterone and estrogen, one must review the above chart showing the major events of the menstrual cycle. Estrogen and progesterone are natural human hormones produced in harmony by the ovary. Estrogen is produced throughout most of the month, from days 5-26 with a peak just before ovulation (day 11) and another peak around day 19.
The Corpus Luteum
Progesterone is produced the last two weeks of the monthly cycle by the corpus luteum, a specialized ovarian structure, representing the remnant of the ovulatory follicle after ovulation. During ovulation, the egg (aka ovum, oocyte) is expelled from the ovarian follicle, and starts its long journey down the fallopian tube to the endometrial cavity where fertilization and implantation may occur (aka ovulation). Ovulation usually occurs on day 11 (vertical dotted line on chart), so progesterone levels start rising on day 12, peaking on day 19-20 or so.
Sudden Decline in Hormone Levels Leads to Bleeding
Both progesterone and estrogen levels decline suddenly around day 26 of the menstrual cycle. This sudden drop in hormone levels initiates menstrual bleeding, the endometrial lining has lost hormonal support and sloughs off (aka menstrual bleeding). Left image shows microscopic view of ovary and corpus luteum courtesy of UNSW Embryology.
Idealized Normal Menstrual Cycle
The above schematic diagram shows the idealized menstrual cycle in the normal female. Firstly, look at the top row. The yellow do-nut like-structure is the corpus luteum in the ovary which makes progesterone. The next row down is body temperature which spikes up at the time of ovulation around day 11. The vertical dotted line represents ovulation around day 11. The next row down we see that FSH and LH spike at the time of ovulation. These are pituitary hormones. FSH is follicle stimulating hormone, and LH is leutinizing hormone. The next row down, we see charts of serum estrogen (yellow) and progesterone (purple). Estrogen spikes just before ovulation, and then has a second peak around day 19. Progesterone starts rising after ovulation, peaks around day 19 and then falls off around day 26. The bottom row shows a schematic of the endometrial lining which thickens with hormonal stimulation, and then sloughs off as hormone levels drop off at day 26.
Anovulation, Estreogen Dominance and Menstrual Irregularities
The chart shows a normal ovulatory cycle. What happens if ovulation does not occur? This is called anovulation, a common problem in young women. in which the ovum is not expelled, no corpus luteum is formed, and no progesterone is produced. Without ovulation, menstrual bleeding becomes irregular, and the cycle length is variable. This leads to a condition known as “estrogen dominance” in which body tissues respond to estrogenic stimulation without progesterone to counter act the estrogen..
PMS – PreMenstrual Syndrome – Estrogen Dominance
Estrogen causes fluid retention and breast tissue stimulation. In the absence of enough progesterone to counter balance the estrogen, the patient may experience bloating, breast enlargement and tenderness, and fluid retention. Estrogen also causes psycho-stimulation, so the patient may complain of insomnia and mood disorders, migraine headaches etc.. As estrogen levels drop, the serum binding protein levels also drop, thus liberating testosterone to cause acne, oily skin and aggressive, “snappy” behavior.
In some cases, ovulation occurs , yet progesterone production is insufficient to balance the massive amounts of estrogen. Similarly these patients suffer from “estrogen dominance” and a similar symptom complex also called “PMS”. premenstrual syndrome.
Treatment for PMS and Irregular Menstrual Cycles
Since progesterone is the missing or deficient element in the PMS syndrome, it would be logical to assume providing progesterone in the form of creams or capsules would benefit the patient. In fact, many doctors and patients report dramatic resolution of PMS symptoms with progesterone capsules and creams. Of course, an annual pelvic exam by the local gynecologist as well as pelvic sonogram is warranted for pre-menopausal women prior to treatment with natural progesterone. Although we will typically perform laboratory testing of hormone levels on day 19 of the menstrual cycle, this type of lab testing is not required by mainstream medicine, and in fact rarely done for treatment of PMS or irregular menstrual bleeding. For more on this, see my article on the importance of the pelvic sonogram.
Still Not Accepted by Mainstream Medicine
Although progesterone is an FDA approved drug, mainstream medicine has yet to accept bioidentical natural human progesterone as a treatment for PMS and irregular menstrual cycles. Instead, mainstream medicine relies on synthetic forms of progesterone called “progestins” such as medroxyprogesteron (Provera) which was shown to cause breast cancer and heart disease in the ill fated Women’s Health Initiative Study. Why hasn’t mainstream medicine accepted progesterone as a valid treatment for PMS? This is explained by the “War Against Natural Medicine”.
The War Against Natural Medicine
In my first book, Natural medicine 101, I delved into the reasons for the information war between natural medicine and mainstream medicine. In short, mainstream medicine is dominated by the drug industry whose profits are dependent on the patented drug system. A patented drug is a natural molecule whose chemical structure has been altered in order to obtain a patent. Molecular structures naturally occurring in the human body or in nature by definition cannot be patented, and are therefore of no interest to the drug industry. Rather, these natural substances such as progesterone represent economic competition to the patented counterparts. That is why progesterone has not taken its rightful place in mainstream medicine treatment of PMS. Left Image courtesy of SheKnows Left image courtesy of Dysfunctional uterine bleeding.
John R Lee MD and Uzzi Reiss M
Thanks and credit goes to Uzzi Reiss MD and John R Lee MD, Most of the material in this article can be found in John R Lees’ chapter on progesterone in his book, What the doctor wont tell you about premenopause. Also Uzzi Reiss’s chapter on progesterone and PMS from his book, Natural Superwoman was another source for this article.
Jeffrey Dach MD
7450 Griffin Road
Suite 180/190
Davie, Florida 33314
954-792-4663
Links and References:
Progesterone FDA Approval Prevention Endometrial Hyperplasia
Mood Biochemistry of Women at Mid-life Phyllis Bronson 2001 J Ortho Mol Med
progesterone Katharina Dalton MD
Conservative management of endometrial hyperplasia Childs OBG MANAGEMENT 2003 Childs, A. J., W. E. Check, and W. J. Hoskins. “Conservative management of endometrial hyperplasia: New strategies, experimental options.” OBG MANAGEMENT 15.9 (2003): 15-26.
Progesterone for Symptomatic Perimenopause Prior 2011 Prior, J. C. “Progesterone for Symptomatic Perimenopause Treatment–Progesterone politics, physiology and potential for perimenopause.” Facts, Views & Vision in ObGyn 3.2 (2011): 109.
Natural progesterone Jane Murray Womens Health Primary Care 1998 Murray, Jane L. “Natural progesterone: what role in women’s health care.” Women’s Health Primary Care 1.8 (1998): 671-87.
progesterone_booklet Lawley Pharmaceuticals 2010
Estrogen carcinogenesis in breast cancer James Yager New England Journal of Medicine 2006
Dose dependent effects oral progesterone oestrogenised postmenopausal endometrium Lane BMJ 1983
Oral micronized progesterone de Lignières Clinical therapeutics 1999 de Lignières, Bruno. “Oral micronized progesterone.” Clinical therapeutics 21.1 (1999): 41-60.
Premenstrual Syndrome Chart American Family Physician
Endometrial_Hyperplasia_Progesterone_ACOG_Brochure
——————————–
http://www.thelancet.com/pdfs/journals/lancet/PIIS0140673604173005.pdf
Katharina Dorothea Dalton
A gynaecologist who popularised the concept of premenstrual syndrome and wrote the best- selling book Once a Month. . Born in London, UK, on Nov 11, 1916, she died on Sept 17, 2004, aged 87 years
Letter containing basic incorrect statements about progesterone
http://www.bmj.com/rapid-response/2011/10/30/katharina-dalton-and-progesterone-dangers
Obituaries Katharina Dorothea Dalton
BMJ 2004; 329 doi: http://dx.doi.org/10.1136/bmj.329.7473.1048-b (Published 28 October 2004) Cite this as: BMJ 2004;329:1048
Removal of the ovaries has long been used to prevent endogenous progesterone production as a treatment for breast cancer. Recent studies confirm that progesterones cause more breast cancer than oestrogens. Progesterone is also potentially teratogenic.
——————————————————–
Freeman, ELLEN W., et al. “A placebo‐controlled study of effects of oral progesterone on performance and mood.” British journal of clinical pharmacology 33.3 (1992): 293-298.
http://www.drkaslow.com/html/progesterone.html
Jeremy E. Kaslow, MD, FACP, FACAAI Physician and Surgeon
Board Certified Internal Medicine
Hormones and the Menstrual Cycle
http://www.ncbi.nlm.nih.gov/pubmed/8726605
Pharmacotherapy. 1996 May-Jun;16(3):453-7.
Oral administration of micronized progesterone: a review and more experience.
McAuley JW1, Kroboth FJ, Kroboth PD.
Historically, oral progesterone has been regarded clinically ineffective because of its poor absorption and rapid clearance. Recent evidence suggests that an oral micronized form of natural progesterone is readily absorbed, produces luteal phase serum concentrations, provokes an end-organ response, and has no detrimental effect on the lipoprotein profile. Thus it is considered by many to be an attractive alternative to synthetic progestin. We evaluated the effects of a single oral dose of micronized progesterone 300 mg in eight healthy postmenopausal women. The maximum serum concentration ranged from 15.72-625.98 ng/ml.
http://www.ncbi.nlm.nih.gov/pubmed/7473442
Efficacy of oral micronized progesterone in the treatment of luteal phase defects.
Frishman GN1, Klock SC, Luciano AA, Nulsen JC.
Vaginal progesterone suppositories are an accepted treatment for infertility attributed to luteal phase defects. Although oral micronized progesterone may be preferable to suppositories for many patients, there are no studies on its use for patients with luteal phase defects. This study evaluated the efficacy of oral micronized progesterone for the treatment of luteal phase defects.
STUDY DESIGN: Seven women with luteal phase defects previously corrected by vaginal suppositories were administered oral micronized progesterone (200 mg by mouth three times a day). Endometrial biopsies were performed to evaluate treatment efficacy. Questionnaires were used to assess side effects, including sedation.
RESULTS: On oral micronized progesterone, all patients had in-phase endometrial biopsies. Despite complaints of drowsiness, the majority of patients preferred the oral formulation over the vaginal route of administration.
CONCLUSION: We conclude that oral micronized progesterone is efficacious in the treatment of luteal phase defects.
http://www.bmj.com/content/287/6401/1241.short
Dose dependent effects oral progesterone oestrogenised postmenopausal endometrium Lane, G., et al. “Dose dependent effects of oral progesterone on the oestrogenised postmenopausal endometrium.” BMJ 287.6401 (1983): 1241-1245.
Full free- BEST
http://www.fertstert.org/article/S0015-0282%2899%2900272-1/fulltext
Fitzpatrick, Lorraine A., and Andrew Good. “Micronized progesterone: clinical indications and comparison with current treatments.” Fertility and sterility 72.3 (1999): 389-397.
Objective: To integrate and evaluate the pharmacokinetic, endocrine, and clinical effects of micronized progesterone formulations.
Design: Published articles concerning the pharmacokinetics of orally administered progesterone and the potential clinical uses of oral micronized progesterone were reviewed. Results concerning their use for secondary amenorrhea, premenopausal bleeding disorders, luteal phase dysfunction, termination of premature labor, hormone replacement therapy, and premenopausal syndrome are summarized. Critical issues to be resolved through ongoing preclinical and clinical research are highlighted.
Result(s): Because of the enhanced bioavailability of oral micronized progesterone, the compound may be useful for a variety of therapeutic indications. Oral micronized progesterone is available in France, and a formulation recently has been approved in the United States for the treatment of secondary amenorrhea and postmenopausal hormone replacement therapy. A large body of evidence, including the Postmenopausal Estrogen/Progestin Interventions study, suggests that the use of a combination of estrogen and oral micronized progesterone is optimal for long-term hormone replacement therapy. There also are data indicating that oral micronized progesterone could be of potential use for the treatment of premenopausal bleeding disorders, luteal phase disorders, and premature labor.
Conclusion(s): Oral micronized progesterone has widespread clinical potential, particularly for the treatment of secondary amenorrhea and dysfunctional premenopausal bleeding, and as a component of postmenopausal hormone replacement therapy.
In summary, oral micronized progesterone has the potential for widespread clinical utility. For indications in which oral delivery of the synthetic progestins currently are used, the theoretic benefits of oral delivery of the natural form of the hormone are obvious. In addition to the decreased potential for adverse effects, there are clear advantages in convenience, cost, compliance, and quality of life.
Acknowledgements
———————————–
Li, Quanxi, et al. “The antiproliferative action of progesterone in uterine epithelium is mediated by Hand2.” Science (New York, Ny) 331.6019 (2011): 912.
P counteracts E-induced endometrial hyperplasia.
pdf available
Munro, Malcolm G., et al. “medroxyprogesterone for acute uterine bleeding Munro Oral medroxyprogesterone acetate and combination oral contraceptives for acute uterine bleeding: a randomized controlled trial.” Obstetrics & Gynecology 108.4 (2006): 924-929.
Bitzer, Johannes, et al. “Medical Management of Heavy Menstrual Bleeding: A Comprehensive Review of the Literature.” Obstetrical & gynecological survey 70.2 (2015): 115-130.
Quinn, Stephen, and Jenny Higham. “Available management options for heavy menstrual bleeding.” Prescriber 25.18 (2014): 18-25.
Matteson, Kristen A., et al. “Nonsurgical management heavy menstrual bleeding systematic review Nonsurgical management of heavy menstrual bleeding: a systematic review.” Obstetrics & Gynecology 121.3 (2013): 632-643.
Matteson, Kristen A., et al. “Practice patterns and attitudes about treating abnormal uterine bleeding: a national survey of obstetricians and gynecologists.” American journal of obstetrics and gynecology 205.4 (2011): 321-e1.
Kaunitz, A. M., et al. “Levonorgestrel-releasing intrauterine system or medroxyprogesterone for heavy menstrual bleeding: a randomized controlled trial.” Obstetrics and gynecology 116.3 (2010): 625.
Managing acute heavy menstrual bleeding
Recommendations for hormonal regimens to halt blood loss in the outpatient
January 01, 2014 By Anita L. Nelson, MD
Aksu, M. Feridun, et al. “High‐Dose Medroxyprogesterone Acetate for the Treatment of Dysfunctional Uterine Bleeding in 24 Adolescents.” Australian and New Zealand journal of obstetrics and gynaecology 37.2 (1997): 228-231.
———————————————————————–
PMS
Once a Month: Understanding and Treating PMS Paperback – March 23, 1999 Katharina Dalton (Author)
http://www.johnleemd.com/store/drphil_anderson.html
Dr. Phil Interview with Holly Anderson: Treating PMS Symptoms With Natural Progesterone . The treatment that works is vaginal or rectal natural progesterone. [Progesterone cream works just as well or better because it’s not messy and drippy! It is delivered to cells throughout the body within minutes of application.] Oral [pill] progesterone does not work for PMS. […because it stresses the liver and creates a lot of metabolites or byproducts, and also only delivers about 20 percent of the dose to the cells].
http://www.aafp.org/afp/2003/0415/p1743.html
Premenstrual Daily Symptom Diary.
Premenstrual Syndrome
LORI M. DICKERSON, PHARM.D., PAMELA J. MAZYCK, PHARM.D., and MELISSA H. HUNTER, M.D., Medical University of South Carolina, Charleston, South Carolina. Am Fam Physician. 2003 Apr 15;67(8):1743-1752.
http://www.ncbi.nlm.nih.gov/pubmed/3924191
Br Med J (Clin Res Ed). 1985 Jun 1;290(6482):1617-21.
Progesterone and the premenstrual syndrome: a double blind crossover trial.
Dennerstein L, Spencer-Gardner C, Gotts G, Brown JB, Smith MA, Burrows GD.
A double blind, randomised, crossover trial of oral micronised progesterone (two months) and placebo (two months) was conducted to determine whether progesterone alleviated premenstrual complaints. Twenty three women were interviewed premenstrually before treatment and in each month of treatment. They completed Moos’s menstrual distress questionnaire, Beck et al’s depression inventory, Spielberger et al’s state anxiety inventory, the mood adjective checklist, and a daily symptom record. Analyses of data found an overall beneficial effect of being treated for all variables except restlessness, positive moods, and interest in sex. Maximum improvement occurred in the first month of treatment with progesterone. Nevertheless, an appreciably beneficial effect of progesterone over placebo for mood and some physical symptoms was identifiable after both one and two months of treatment. Further studies are needed to determine the optimum duration of treatment.
http://www.amazon.com/Emerita-Pro-Gest-Cream-tube-PACKAGING/product-reviews/B000IMQE5U
Emerita Pro-Gest Cream, 4 oz. tube (PACKAGING MAY VARY)
byEmerita on Amazon
http://www.drnorthrup.com/heavy-menstrual-bleeding-menorrhagia/
Heavy Menstrual Bleeding (Menorrhagia) Christiane Northrup, M.D.
Although I prefer to try natural progesterone first, if that doesn’t work, a strong synthetic progestin such as medroxyprogesterone acetate (Provera) can help. (This is the only circumstance in which I recommend the synthetic.) T – See more at: http://www.drnorthrup.com/heavy-menstrual-bleeding-menorrhagia/#sthash.6GlJCGzW.dpuf
http://www.pmstreatmentclinic.com/services.html
PMS Treatment Clinic using bioidentical hormones to treat premenstrual syndrome.
Treatment of Premenstrual Syndrome
Premenstrual Syndrome is a condition of estrogen dominance-progesterone deficiency. It occurs in the two weeks before the period and goes away when the period is over. 150 emotional and physical symptoms can occur. Symptoms may include headaches, migraines, menstrual cramps, depression, irritability, fatigue, emotional outbursts, low blood sugar, rage, out of control behavior, dizziness, decreased resistance to infection and epileptic seizures. An underactive thyroid is commonly an underlying disorder that is present.
Patients can become symptom-free on natural progesterone therapy. If the patient is hypothyroid, treatment involves thyroid supplements.
https://www.womentowomen.com/pms/severe-pms-and-pmdd-treatment/
by Marcelle Pick, OB/GYN NP
Advanced Premenstrual Syndrome (PMS) and Premenstrual Dysphoric Disorder (PMDD) Treatment
http://www.womenlivingnaturally.com/articlepage.php?id=29
Dysfunctional Uterine Bleeding
http://www.georgiahormones.com/Progesterone-Use-For-Cycle-Regulation.aspx
Progesterone Use for Cycle Regulation
If you are reading this flyer, it is likely that you are having problems with irregular, heavy or abnormal periods and have been given a prescription for Progesterone supplementation. The most common cause of these problems is irregular or inadequate production of progesterone.
============================================================
http://www.mountainspringsmedicine.com/14.html
UNOPPOSED ESTROGEN AND THE PERI-MENOPAUSAL TRANSITION
http://press.endocrine.org/doi/abs/10.1210/edrv.21.1.0386
Is Estradiol a Genotoxic Mutagenic Carcinogen? Joachim G. Liehr July 01, 2013 Endocrine Reviews
Yager, James D., and Nancy E. Davidson. “Estrogen carcinogenesis in breast cancer.” New England Journal of Medicine 354.3 (2006): 270-282.
Campagnoli, Carlo, et al. “Progestins and progesterone in hormone replacement therapy and the risk of breast cancer.” The Journal of steroid biochemistry and molecular biology 96.2 (2005): 95-108.
The post Progesterone for PMS Part Two appeared first on Jeffrey Dach MD .
For part one
click here.









Leave a Comment
You must be logged in to post a comment.