 Vitamin K, Is There Anything It Can’t Do ?
Vitamin K, Is There Anything It Can’t Do ?
Back in the old days (1972-1976) we made rounds every morning on the medical ward at the University of Illinois Hospital. A 5 mg vitamin K injection was commonly ordered for liver disease patients who had bleeding disorders from inability to manufacture clotting factors.
Another 3 month rotation was on the surgical floor where I found the surgeons pacing impatiently whenever their procedures where delayed. This was usually due to an abnormal coagulation profile, usually from blood thinner medication, warfarin, which antagonizes Vitamin K and inhibits hepatic production of clotting factors. A vitamin K injection promptly restores the coagulation factors, and the procedure can proceed promptly, and the surgeons stop their pacing back and forth.
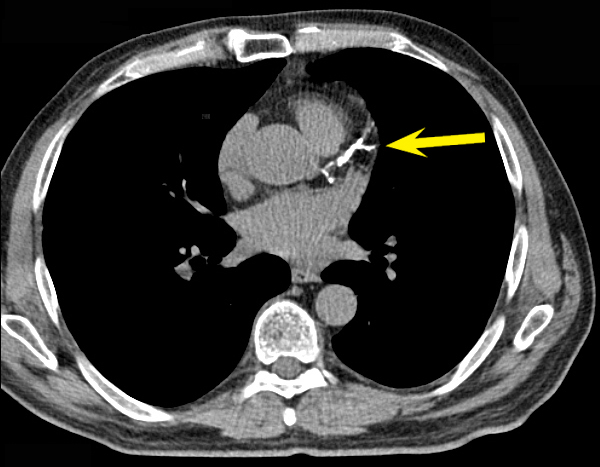
(Warfarin_Vitamin_K_Patel_2008 ) Above left image calcified coronary artery on CAT scan courtesy of Cedars Sinai Edu.
More Than Just Clotting Factors
New research into cell physiology over the last two decades shows the Koagulation Vitamin has other more extensive activities. Vitamin K is involved in the activation of Vitamin K-dependent (VKD) proteins which are “carboxylated” rendering VKD proteins active in roles that include “hemostasis, apoptosis, bone mineralization, calcium homeostasis, growth control, and signal transduction”.
Further studies show that although we may have sufficient vitamin intake to prevent bleeding disorders, because of the “Triage Effect” described by Vermeer, we have have insufficient Vitamin K intake to prevent degenerative diseases of aging, atherosclerosis with arterial calcification, osteoporosis, and cancer.
“It seems, however, that our dietary vitamin K intake is too low to support the carboxylation of at least some of these Gla-proteins. According to the triage theory, long-term vitamin K inadequacy is an independent, but modifiable risk factor for the development of degenerative diseases of ageing including osteoporosis and atherosclerosis.(reference: Vermeer)
Soft Tissue and Coronary artery calcification
It is well known based on clinical experience alone, that Warfarin, a vitamin K antagonist increases soft tissue and arterial calcifications. Human studies confirm increased extra-coronary artery calcification induced by warfarin, an effect reversible with high Vitamin K intake. An association between low Vitamin K intake and increased risk for coronary artery disease was found in the Rotterdam Study (1-5).
Discordant Calcium Scoring Studies
Calcium scoring studies in patient on warfarin are discordant, and have so far shown no increased coronary artery calcification from warfarin use. I suspect, something went wrong with these studies. Perhaps the control patients had enough vitamin K deficiency to allow them to form coronary artery calcification same as the Warfarin treated group. Later studies looking at Matrix GLA protein as a marker for Vitamin K status good correlation as as one might expect as we discuss below.. (see below)
In addition, further studies looking at serial calcium scores shows reduced progression of calcium score in Vitamin K treated patients, as one might expect. (Kyla Shea) Thus, we have a recommendation for Vitamin K as part of a program to reduce calcium score, and reduce risk for Heart Attack.
 Concordant Calcium Scoring Studies
Concordant Calcium Scoring Studies
A number of excellent studies were done by Drs Vermeer et al. from the Netherlands showed excellent correlation between calcium score, heart disease risk, mortality from heart disease and uncarboxylated Matrix GLA protein, the best marker for Vitamin K deficiency.
An excellent Calcium Scoring study by Drs Vermeer and Rennenberg showed good correlation between calcium score and Vitamin K status. Remember the role of vitamin K, which is an essential cofactor to carboxylate matrix Gla protein, itself a potent inhibitor of vascular calcification. Dr Vermeer et al found the calcium score was significantly associated with ucMGP (uncarboxylarted Matrix GLA, an indicator of Vitamin K deficiency).(11) Another Vermeer study published in 2014, again showed a more than two fold increase in cardiovascular risk for elderly men and women with lower vitamin K status as measured by the uncarboxylated MGP marker.
Another Vermeer study published in Atherosclerosis July 2014, again showed more than doubling of mortality in the low vitamin K group. This study followed 800 people for 5 years with a mean age of 65 , all with known cardiovascvular . Patient in the highest quartile for uncarboxylated Matrix GLA (uMGLA), a marker for low vitamin K status, had almost double the mortality from cardiovascular disease.
Vitamin D Intake
Further studies show that Vitamin D intake accelerates soft tissue calcification in the presence of Vitamin K deficiency, or a Vitamin K antagonist such as Warfarin. Calcium supplementation as you might expect, increases the risk for myocardial infarction.(Bolland) Underlying vitamin K deficiency, in a patient taking vitamin D and calcium to prevent osteoporosis is the likely underlying scenario at play here.
Preventing Cancer
Another surprising benefit of Vitamin K is as a cancer preventive. A number of cell culture and animal xenograft studies shows that vitamin K2 induces “Apoptosis” (programmed cell death) in cancer cells.(12-21) There were a number of different cancers studied including Glioblastoma, Hepatocellular Cancer, Lung Cancer, Prostate Cancer, etc.(12-21) Based on these reports, one might suggest adding Vitamin K2 to a supplement program for anyone seeking to prevent cancer, or cancer recurrence after treatment.
Vitamin K for Rheumatoid Arthritis: Another study shows Vitamin K is useful as a treatment for Rhematoid arthritis. (22)
Vitamin K for Bones
For women taking Calcium and Vitamin D to maintain strong bones and preventing osteoporosis, vitamin K is especially important. In the past few years, many bone calcium supplement companies have added Vitamin K to upgrade their Calcium and Vitamin D product. Many of these brands are reviewed by Consumer Reports, including Adora, Allergy Research Group, Caltrate, Carlson, Citracal, DaVinci Laboratories of Vermont, Floradix, Garden of Life, GNC, Isotonix (Market America), Julian Whitaker MD, Kirkland (Costco), Lifetime, Li’l Critters, Nature’s Bounty, Nature Made, Nature’s Plus, Nature’s Life, Nutrition Now, OSCal, Puritan’s Pride, Physiologics, Pure Encapsulations, Quest, Rite Aid, Standard Process, Sundown, Trader Darwin’s (Trader Joe’s), Twinlab, Vitamin Shoppe, and Vitamin World.
Vitamin K strengthens our bones, increases bone mineral density BMD, and reduces fracture risk. Retrospective studies of Vitamin K antagonists, coumarin type blood thinners suggest an adverse affect on vertebral BMD and fracture risk.(24)
In a randomized trial. Vermeer tested whether high vitamin K2 intake promotes bone mineral density and bone strength. His results showed that K2 improved bone mineral content BMC and femoral neck width, but not bone mineral density by DEXA scan (25)
Buy Vitamin K2 on Amazon
Buy Synergy K on PureCaps
Recommended Reading: Vitamin K2 and the Calcium Paradox
Link to this article:http://wp.me/p3gFbV-281
Jeffrey Dach MD
7450 Griffin Road, Suite 190
Davie, Fl 33314
954-792-4663
http://www.jeffreydachmd.com
http://www.drdach.com
http://www.naturalmedicine101.com
http://www.bioidenticalhormones101.com
References and Links
vitamin K and Coronary artery calcification, soft tissue calcification
1) http://www.ncbi.nlm.nih.gov/pubmed/8698544
Int J Vitam Nutr Res. 1996;66(1):36-8.
Effect of vitamin K2 on experimental calcinosis induced by vitamin D2 in rat soft tissue.Seyama Y, Horiuch M, Hayashi M, Kanke Y.
Source Dept. of Clinical Chemistry, Hoshi College of Pharmacy, Tokyo, Japan.Abstract The effect of vitamin K2 on calcium (Ca) and inorganic phosphorus (P) levels in the aorta and kidney obtained from experimental calcinosis induced by vitamin D2(2.5 x 10(5) I.U./ kg b.w.) of male rats was investigated.
A high dose of vitamin K2 (100 mg/kg b.w.) inhibited the increase in the aortic Ca and P or in the renal Ca and P induced by vitamin D2, and a low dose of vitamin K2 (10 mg/kg b.w.) showed the same tendency, but the degree of the efficacy was small. It may be suggested that a high dose of vitamin K2 suppressed experimental calcification of soft tissues induced by vitamin D2. Therefore, a pharmacological dose of vitamin K2 might have a usefulness for the prevention and treatment of arteriosclerosis with calcification.
2)www.ncbi.nlm.nih.gov/pubmed/9414028
Jpn J Pharmacol. 1997 Oct;75(2):135-43.
Effects of vitamin K2 (menatetrenone) on atherosclerosis and blood coagulation in hypercholesterolemic rabbits.
Kawashima H, Nakajima Y, Matubara Y, Nakanowatari J, Fukuta T, Mizuno S, Takahashi S, Tajima T, Nakamura T. Source Pharmacological Evaluation Section, Tokyo Research Laboratoires, Eisai Co., Ltd., Koishikawa, Japan.
Abstract Gamma-Carboxyglutamic acid (Gla)-containing protein, synthesized in the presence of vitamin K, has been found in atherogenic plaques, but the pharmacological effect of vitamin K on atherosclerosis is unclear.
We examined whether vitamin K2 (menatetrenone) could affect the progression of both atherosclerosis and hypercoagulability in hypercholesterolemic rabbits. Vitamin K2 in daily doses of 1, 10 and 100 mg/kg was given with a 0.5% cholesterol diet for 10 weeks to 8 rabbits each. The plasma levels of total-cholesterol in the vitamin K2-treated groups were clearly lower than that of the hypercholesterolemic control group. The excessive dose of vitamin K2, even at the high dose of 100 mg/kg/day for 10 weeks, did not accelerate the progression of atherosclerosis and did not promote the coagulative tendency in the rabbits.
In contrast, the vitamin K2 treatment (1 to 10 mg/kg/day) suppressed the progression of atherosclerotic plaques, intima-thickening and pulmonary atherosclerosis, the increase of ester-cholesterol deposition in the aorta, and both the elevation in plasma factor X level and increase in Hepaplastin test value in the rabbits. These results indicate that the pharmacological dose of vitamin K2 prevents both the progression of atherosclerosis and the coagulative tendency by reducing the total-cholesterol, lipid peroxidation and factor X activity in plasma, and the ester-cholesterol deposition in the aorta in hypercholesterolemic rabbits.
3) http://www.ncbi.nlm.nih.gov/pubmed/18722618
Atherosclerosis. 2009 Apr;203(2):489-93. Epub 2008 Jul 19.
High dietary menaquinone intake is associated with reduced coronary calcification.
Beulens JW, Bots ML, Atsma F, Bartelink ML, Prokop M, Geleijnse JM, Witteman JC, Grobbee DE, van der Schouw YT.
Source Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, The Netherlands. J.Beulens@umcutrecht.nl
Abstract BACKGROUND: Dietary vitamin K is thought to decrease risk of cardiovascular disease by reducing coronary calcification, but inconsistent results are reported. This may be due to different effects of vitamin K(1) (phylloquinone) and vitamin K(2) (menaquinone, MK), but few studies included both.
METHODS: We investigated the association of intake of phylloquinone and menaquinone, including its subtypes (MK4-MK10), with coronary calcification in a cross-sectional study among 564 post-menopausal women. Phylloquinone and menaquinone intake was estimated using a food-frequency questionnaire.
RESULTS: Sixty-two percent (n=360) of the women had coronary calcification based on 1.5-mm thick slices. Phylloquinone intake was not associated with coronary calcification with a relative risk (RR) of 1.17 (95%-confidence interval: 0.96-1.42; p(trend)=0.11) of the highest versus lowest quartile. Menaquinone intake was associated with decreased coronary calcification with an RR of 0.80 (95%-CI: 0.65-0.98; p(trend)=0.03).CONCLUSION: This study shows that high dietary menaquinone intake, but probably not phylloquinone, is associated with reduced coronary calcification. Adequate menaquinone intakes could therefore be important to prevent cardiovascular disease.
4) http://www.ncbi.nlm.nih.gov/pubmed/19179058
Nutr Metab Cardiovasc Dis. 2009 Sep;19(7):504-10. Epub 2009 Jan 28.
A high menaquinone intake reduces the incidence of coronary heart disease. Gast GC, de Roos NM, Sluijs I, Bots ML, Beulens JW, Geleijnse JM, Witteman JC, Grobbee DE, Peeters PH, van der Schouw YT.Source Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, 3508 GA Utrecht, The Netherlands.
Abstract BACKGROUND AND AIM: Vitamin K dependent proteins have been demonstrated to inhibit vascular calcification. Data on the effect of vitamin K intake on coronary heart disease (CHD) risk, however, are scarce. To examine the relationship between dietary vitamins K(1) and K(2) intake, and its subtypes, and the incidence of CHD.
METHODS AND RESULTS: We used data from the Prospect-EPIC cohort consisting of 16,057 women, enrolled between 1993 and 1997 and aged 49-70 years, who were free of cardiovascular diseases at baseline. Intake of vitamin K and other nutrients was estimated with a food frequency questionnaire. Multivariate Cox proportional hazards models were used to analyse the data. After a mean+/-SD follow-up of 8.1+/-1.6 years, we identified 480 incident cases of CHD. Mean vitamin K(1) intake was 211.7+/-100.3 microg/d and vitamin K(2) intake was 29.1+/-12.8 microg/d. After adjustment for traditional risk factors and dietary factors, we observed an inverse association between vitamin K(2) and risk of CHD with a Hazard Ratio (HR) of 0.91 [95% CI 0.85-1.00] per 10 microg/d vitamin K(2) intake. This association was mainly due to vitamin K(2) subtypes MK-7, MK-8 and MK-9. Vitamin K(1) intake was not significantly related to CHD. CONCLUSIONS: A high intake of menoquinones, especially MK-7, MK-8 and MK-9, could protect against CHD. However, more research is necessary to define optimal intake levels of vitamin K intake for the prevention of CHD.
Cees Vermeer 2012
5) Prolonged sub-clinical vitamin K deficiency is a risk factor for osteoporosis, atherosclerosis, and cancer.
http://www.ncbi.nlm.nih.gov/
http://www.ncbi.nlm.nih.gov/
Food Nutr Res. 2012;56. Vitamin K: the effect on health beyond coagulation – an overview. Vermeer C. VitaK and Cardiovascular Research Institute CARIM, Maastricht University, Maastricht, The Netherlands.
Vitamin K is essential for the synthesis of proteins belonging to the Gla-protein family. To the members of this family belong four blood coagulation factors, which all are exclusively formed in the liver. The importance of vitamin K for hemostasis is demonstrated from the fact that vitamin K-deficiency is an acute, life-threatening condition due to excessive bleeding. Other members of the Gla-protein family are osteocalcin, matrix Gla-protein (MGP), and Gas6 that play key functions in maintaining bone strength, arterial calcification inhibition, and cell growth regulation, respectively. In total 17 Gla-proteins have been discovered at this time. Recently, it was observed that the dietary vitamin K requirement for the synthesis of the coagulation factors is much lower than for that of the extra-hepatic Gla-proteins. This forms the basis of the triage theory stating that during poor dietary supply, vitamins are preferentially utilized for functions that are important for immediate survival. This explains why in the healthy population all clotting factors are synthesized in their active form, whereas the synthesis of other Gla-proteins is sub-optimal in non-supplemented subjects. Prolonged sub-clinical vitamin K deficiency is a risk factor for osteoporosis, atherosclerosis, and cancer. Present recommendations for dietary intake are based on the daily dose required to prevent bleeding. Accumulating scientific data suggests that new, higher recommendations for vitamin K intake should be formulated.
Risk factor for cardiovascular morbidity and mortality
After extensive databases had been constructed for the vitamin K1- and vitamin K2-content of various food items, population-based studies were initiated to correlate vitamin K intake with cardiovascular disease. In a first survey, Geleijnse et al. (11) demonstrated that vitamin K2 intake is inversely correlated with cardiovascular disease and mortality. Remarkably, no association was found with the intake of vitamin K1. The study was a 10-year follow-up of 4,500 elderly subjects (the Rotterdam study cohort) with a highest quartile for K2 intake of 45
µg/day. These data were confirmed by Gast et al. (12) in over 16,000 participants of the Prospect study. Because of the large number of subjects and the long follow-up period, the effects of individual menaquinones could be tested. Long-chain menaquinones (MK-7 and higher) turned out to have the most beneficial effects on cardiovascular disease, with a mortality risk reduction of 9% for each 10 µg/day of extra intake. These outcomes prompted us to develop a more direct test for vascular vitamin K status and obviously circulating MGP was the target biomarker for such test.
Poor vitamin K status was also found to be associated with low bone mass, osteoporosis, and fracture risk
Secondary (or sub-clinical) vitamin K deficiency would then form an increased risk factor for accelerated bone loss, vascular calcification, and cancer. Indeed all these associations have been reported in the literature (8, 17, 20).
—————
Vitamin K references
Vermeer
6) http://www.ncbi.nlm.nih.gov/
Menopause Int. 2011 Mar;17(1):19-23.
Vitamin K, osteoporosis and degenerative diseases of ageing.
Vermeer C1, Theuwissen E. 1VitaK, Maastricht University, Oxfordlaan 70, 6229 EV Maastricht, The Netherlands.
The function of vitamin K is to serve as a co-factor during the post-translational carboxylation of glutamate (Glu) residues into γ-carboxyglutamate (Gla) residues. The vital importance of the Gla-proteins essential for normal haemostasis is well recognized. During recent years, new Gla-containing proteins have been discovered and the vitamin K-dependent carboxylation is also essential for their function. It seems, however, that our dietary vitamin K intake is too low to support the carboxylation of at least some of these Gla-proteins. According to the triage theory, long-term vitamin K inadequacy is an independent, but modifiable risk factor for the development of degenerative diseases of ageing including osteoporosis and atherosclerosis.
7) http://www.ncbi.nlm.nih.gov/
Am J Clin Nutr. 2009 Oct;90(4):889-907. doi: 10.3945/ajcn.2009.27930. Epub 2009 Aug 19. Vitamin K, an example of triage theory: is micronutrient inadequacy linked to diseases of aging? McCann JC1, Ames BN. 1Children’s Hospital Oakland Research Institute, Oakland, CA 94609, USA.
The triage theory posits that some functions of micronutrients (the approximately 40 essential vitamins, minerals, fatty acids, and amino acids) are restricted during shortage and that functions required for short-term survival take precedence over those that are less essential. Insidious changes accumulate as a consequence of restriction, which increases the risk of diseases of aging. For 16 known vitamin K-dependent (VKD) proteins, we evaluated the relative lethality of 11 known mouse knockout mutants to categorize essentiality. Results indicate that 5 VKD proteins that are required for coagulation had critical functions (knockouts were embryonic lethal), whereas the knockouts of 5 less critical VKD proteins [osteocalcin, matrix Gla protein (Mgp), growth arrest specific protein 6, transforming growth factor beta-inducible protein (Tgfbi or betaig-h3), and periostin] survived at least through weaning. The VKD gamma-carboxylation of the 5 essential VKD proteins in the liver and the 5 nonessential proteins in nonhepatic tissues sets up a dichotomy that takes advantage of the preferential distribution of dietary vitamin K1 to the liver to preserve coagulation function when vitamin K1 is limiting.
Genetic loss of less critical VKD proteins, dietary vitamin K inadequacy, human polymorphisms or mutations, and vitamin K deficiency induced by chronic anticoagulant (warfarin/coumadin) therapy are all linked to age-associated conditions: bone fragility after estrogen loss (osteocalcin) and arterial calcification linked to cardiovascular disease (Mgp). There is increased spontaneous cancer in Tgfbi mouse knockouts, and knockdown of Tgfbi causes mitotic spindle abnormalities.
A triage perspective reinforces recommendations of some experts that much of the population and warfarin/coumadin patients may not receive sufficient vitamin K for optimal function of VKD proteins that are important to maintain long-term health.
8) http://www.ncbi.nlm.nih.gov/
J Thromb Haemost. 2004 Dec;2(12):2118-32.
The physiology of vitamin K nutriture and vitamin K-dependent protein function in atherosclerosis. Berkner KL1, Runge KW. 1Department of Molecular Cardiology, Lerner Research Institute, Cleveland Clinic Lerner College of Medicine at Case Western Reserve University, Cleveland, OH 44195, USA.
Recent advances in the discovery of new functions for vitamin K-dependent (VKD) proteins and in defining vitamin K nutriture have led to a substantial revision in our understanding of vitamin K physiology. The only unequivocal function for vitamin K is as a cofactor for the carboxylation of VKD proteins which renders them active. While vitamin K was originally associated only with hepatic VKD proteins that participate in hemostasis, VKD proteins are now known to be present in virtually every tissue and to be important to bone mineralization, arterial calcification, apoptosis, phagocytosis, growth control, chemotaxis, and signal transduction. The development of improved methods for analyzing vitamin K has shed considerable insight into the relative importance of different vitamin K forms in the diet and their contribution to hepatic vs. non-hepatic tissue. New assays that measure the extent of carboxylation in VKD proteins have revealed that while the current recommended daily allowance for vitamin K is sufficient for maintaining functional hemostasis, the undercarboxylation of at least one non-hemostatic protein is frequently observed in the general population. The advances in defining VKD protein function and vitamin K nutriture are described, as is the potential impact of VKD proteins on atherosclerosis. Many of the VKD proteins contribute to atherogenesis. Recent studies suggest involvement in arterial calcification, which may be influenced by dietary levels of vitamin K and by anticoagulant drugs such as warfarin that antagonize vitamin K action.
9) http://www.ncbi.nlm.nih.gov/
Int J Vitam Nutr Res. 1996;66(1):36-8.
Effect of vitamin K2 on experimental calcinosis induced by vitamin D2 in rat soft tissue. * Seyama Y1, Horiuch M, Hayashi M, Kanke Y. 1Dept. of Clinical Chemistry, Hoshi College of Pharmacy, Tokyo, Japan.
The effect of vitamin K2 on calcium (Ca) and inorganic phosphorus (P) levels in the aorta and kidney obtained from experimental calcinosis induced by vitamin D2(2.5 x 10(5) I.U./ kg b.w.) of male rats was investigated. A high dose of vitamin K2 (100 mg/kg b.w.) inhibited the increase in the aortic Ca and P or in the renal Ca and P induced by vitamin D2, and a low dose of vitamin K2 (10 mg/kg b.w.) showed the same tendency, but the degree of the efficacy was small. It may be suggested that a high dose of vitamin K2 suppressed experimental calcification of soft tissues induced by vitamin D2. Therefore, a pharmacological dose of vitamin K2 might have a usefulness for the prevention and treatment of arteriosclerosis with calcification.
10) http://www.ncbi.nlm.nih.gov/
Jpn J Pharmacol. 1997 Oct;75(2):135-43.
Effects of vitamin K2 (menatetrenone) on atherosclerosis and blood coagulation in hypercholesterolemic rabbits. Kawashima H1, Nakajima Y, Matubara Y, Nakanowatari J, Fukuta T, Mizuno S, Takahashi S, Tajima T, Nakamura T.
Gamma-Carboxyglutamic acid (Gla)-containing protein, synthesized in the presence of vitamin K, has been found in atherogenic plaques, but the pharmacological effect of vitamin K on atherosclerosis is unclear. We examined whether vitamin K2 (menatetrenone) could affect the progression of both atherosclerosis and hypercoagulability in hypercholesterolemic rabbits. Vitamin K2 in daily doses of 1, 10 and 100 mg/kg was given with a 0.5% cholesterol diet for 10 weeks to 8 rabbits each. The plasma levels of total-cholesterol in the vitamin K2-treated groups were clearly lower than that of the hypercholesterolemic control group. The excessive dose of vitamin K2, even at the high dose of 100 mg/kg/day for 10 weeks, did not accelerate the progression of atherosclerosis and did not promote the coagulative tendency in the rabbits. In contrast, the vitamin K2 treatment (1 to 10 mg/kg/day) suppressed the progression of atherosclerotic plaques, intima-thickening and pulmonary atherosclerosis, the increase of ester-cholesterol deposition in the aorta, and both the elevation in plasma factor X level and increase in Hepaplastin test value in the rabbits. These results indicate that the pharmacological dose of vitamin K2 prevents both the progression of atherosclerosis and the coagulative tendency by reducing the total-cholesterol, lipid peroxidation and factor X activity in plasma, and the ester-cholesterol deposition in the aorta in hypercholesterolemic rabbits.
11) http://www.ncbi.nlm.nih.gov/pubmed/20486996
Eur J Clin Invest. 2010 Apr;40(4):344-9. doi: 10.1111/j.1365-2362.2010.02275.x.
Calcium scores and matrix Gla protein levels: association with vitamin K status.
Rennenberg RJ1, de Leeuw PW, Kessels AG, Schurgers LJ, Vermeer C, van Engelshoven JM, Kemerink GJ, Kroon AA.
1Department of Internal Medicine, Maastricht University Medical Centre (MUMC+) and Cardiovascular Research Institute Maastricht (CARIM), Maastricht, The Netherlands. r.rennenberg@mumc.nl
Vascular calcification in humans is associated with an increased cardiovascular risk. Carboxylated matrix Gla protein (cMGP) inhibits vascular calcification. Vitamin K is an essential cofactor for the activation of uncarboxylated matrix Gla protein (ucMGP). It has been suggested that patients on long-term treatment with vitamin K antagonists develop aortic valve calcifications because of lower levels of circulating MGP. We therefore hypothesized that arterial calcification and a low vitamin K status are associated with ucMGP. To that aim, we measured arterial calcium scores, the osteocalcin ratio (OCR), as a proxy for vitamin K status, and ucMGP.
MATERIALS AND METHODS: In 36 hypertensive patients, we determined the Agatston score with computer tomography scans of the abdominal aorta, carotid and coronary arteries. The total calcium score was calculated as the sum of the separate Z-scores.
RESULTS: The total calcium Z-score was significantly correlated to age (r = 0.683, P < 0.001), smoking (r = 0.372, P = 0.026), total cholesterol (r = 0.353, P = 0.034), LDL cholesterol (r = 0.490, P = 0.003), triglycerides (r = 0.506, P = 0.002), fasting glucose (r = 0.454, P = 0.005), systolic blood pressure (r = 0.363, P = 0.029) and pulse pressure (r = 0.685, P < 0.001). In multivariate regression analyses, OCR and total calcium score were significantly associated with ucMGP.
CONCLUSIONS: We found a positive association of total arterial calcium score and a high OCR (reflecting low vitamin K status) with ucMGP serum levels. This warrants further studies to explore the pathophysiological background of this phenomenon.
==============================
12)http://www.ncbi.nlm.nih.gov/
Cancer. 2006 Feb 15;106(4):867-72.
The effect of menatetrenone, a vitamin K2 analog, on disease recurrence and survival in patients with hepatocellular carcinoma after curative treatment: a pilot study.
Mizuta T1, Ozaki I, Eguchi Y, Yasutake T, Kawazoe S, Fujimoto K, Yamamoto K.
1Department of Internal Medicine, Saga Medical School, Japan.
The high recurrence rate of hepatocellular carcinoma (HCC) determines the long-term prognosis for patients with HCC. In the current study, the authors tested the effects of menatetrenone, a vitamin K2 analog, on recurrent HCC and survival after curative treatment.
METHODS:Sixty-one patients who were diagnosed as free of HCC after surgical resection or percutaneous local ablation were assigned randomly assigned to either a menatetrenone group (n = 32 patients) or a control group (n = 29 patients). Patients in the menatetrenone group received a daily oral dose of 45 mg of menatetrenone. Disease recurrence and survival rates were analyzed in patients with HCC.
RESULTS:The cumulative recurrence rates in the menatetrenone group were 12.5% at 12 months, 39.0% at 24 months, and 64.3% at 36 months; and the corresponding recurrence rates in the control group were 55.2%, 83.2%, and 91.6%, respectively (P = 0.0002). Similar results were obtained even for patients who had low baseline levels of serum des-gamma-carboxy-prothrombin. Univariate and multivariate Cox proportional hazard analyses showed that the administration of menatetrenone was the only factor related to the recurrence rate of HCC. The cumulative survival rates for the patients who received menatetrenone were 100% at 12 months, 96.6% at 24 months, and 87.0% at 36 months; and the corresponding survival rates for patients in the control group were 96.4%, 80.9%, and 64.0%, respectively (P = 0.051).
CONCLUSIONS:The current study findings suggested that menatetrenone may have a suppressive effect on recurrence of HCC and a beneficial effect on survival, although a larger, placebo-controlled trial will be required to prove these effects.
13)http://www.ncbi.nlm.nih.gov/
PLoS One. 2013;8(3):e58082. doi: 10.1371/journal.pone.0058082. Epub 2013 Mar 7.
Postoperative use of the chemopreventive vitamin K2 analog in patients with hepatocellular carcinoma. Zhong JH1, Mo XS, Xiang BD, Yuan WP, Jiang JF, Xie GS, Li LQ.
1Hepatobiliary Surgery Department, Tumor Hospital of Guangxi Medical University, Nanning, People’s Republic of China.
To evaluate the chemopreventive efficacy of vitamin K2 (VK2) analog in patients with hepatocellular carcinoma (HCC) after curative hepatic resection or local ablation, since a recent randomized control trial (RCT) and systematic review have given contradictory results.
METHODS:MEDLINE, EMBASE and Cochrane library databases were systematically searched through the end of May 2012. Meta-analysis of RCTs and cohort studies was performed to estimate the effects of the VK2 analog on tumor recurrence rate and overall survival (OS). Risk ratios (RRs) and 95% confidence intervals (95% CIs) were calculated.
RESULTS:Six RCTs and one cohort study involving a total of 930 patients were included. VK2 analog therapy did not reduce the 1-year recurrence rate, with a pooled RR of 0.67 (95% CI 0.39-1.13, p = 0.13). However, VK2 analog therapy was associated with a significant reduction in the 2- and 3-year tumor recurrence rates, with respective pooled RRs of 0.65 (95% CI 0.51-0.83, p<0.001) and 0.70 (95% CI = 0.58-0.85, p<0.001). The therapy was also associated with a significant improvement in 1-, 2-, and 3-year OS, with respective pooled RRs of 1.03 (95% CI 1.01-1.05, p = 0.02), 1.11 (95% CI 1.03-1.19, p = 0.005) and 1.14 (95% CI 1.02-1.28, p = 0.02). None of the studies reported adverse effects attributable to VK2 analog therapy.
CONCLUSION:The VK2 analog may reduce recurrence rate after 1 year and improve OS in HCC patients as early as 1 year. However, these findings should be considered preliminary since the majority of patients came from an RCT with survival data out to only 1 year. More extensive studies with larger sample sizes and longer follow-up are needed.
14) http://www.ncbi.nlm.nih.gov/
Int J Oncol. 2005 Aug;27(2):505-11.
Vitamins K2, K3 and K5 exert in vivo antitumor effects on hepatocellular carcinoma by regulating the expression of G1 phase-related cell cycle molecules.
Kuriyama S1, Hitomi M, Yoshiji H, Nonomura T, Tsujimoto T, Mitoro A, Akahane T, Ogawa M, Nakai S, Deguchi A, Masaki T, Uchida N. 1Third Department of Internal Medicine, Kagawa University School of Medicine, Kita-gun, Kagawa 761-0793, Japan.
A number of studies have shown that various vitamins K, specifically vitamin K2, possessed antitumor activity on various types of rodent- and human-derived neoplastic cell lines. However, there are only a small number of reports demonstrating in vivo antitumor effects of vitamins K. Furthermore, the mechanism of antitumor effects of vitamins K still remains to be examined. In the present study, we examined the antitumor effects of vitamins K2, K3 and K5 on PLC/PRF/5 human hepatocellular carcinoma (HCC) cells in vivo. Furthermore, to examine the mechanism of antitumor actions of these vitamins K, mRNA expression levels of various G1 phase-related cell cycle molecules were evaluated by using a real-time reverse transcription-polymerase chain reaction (RT-PCR) method. HCC-bearing animals were produced by implanting PLC/PRF/5 cells subcutaneously into athymic nude mice, and drinking water containing vitamin K2, K3 or K5 was given to the animals. Treatments with vitamins K2, K3 and K5 were shown to markedly inhibit the growth of HCC tumors. To examine the mechanism of in vivo antitumor effects of vitamins K, total RNA was extracted from HCC tumors, and the expression of G1 phase-related cell cycle molecules was quantitatively examined. Real-time RT-PCR demonstrated that the expression of the cell cycle-driving molecule, cyclin-dependent kinase 4 (Cdk4), in HCC was significantly reduced by the treatments with vitamin K2, K3 and K5. Conversely, the expression of the cell cycle-suppressing molecules, Cdk inhibitor p16INK4a and retinoblastoma, in HCC was significantly enhanced by the treatments with vitamins K2, K3 and K5. These results indicate that vitamins K2, K3 and K5 exert antitumor effects on HCC by regulating the expression of G1 phase-related cell cycle molecules. These results also indicate that vitamins K2, K3 and K5 may be useful agents for the treatment of patients with HCC.
15) http://www.ncbi.nlm.nih.gov/
Acta Neurol Belg. 2004 Sep;104(3):106-10.
Comparison of vitamins K1, K2 and K3 effects on growth of rat glioma and human glioblastoma multiforme cells in vitro. Oztopçu P1, Kabadere S, Mercangoz A, Uyar R.
1Osmangazi University Art and Sciences Faculty Department of Biology, Eskişehir, Türkiye.
Glioblastoma multiforme is characterized as highly invasive and rapidly growing astrocytomas, and scientists have sought for efficient treatment against malignant gliomas for a long time. Therefore, we compared the respond of rat glioma (C6) and glioblastoma multiforme cells derived from two patients to vitamins K1, K2 and K3. The cells were exposed to 100, 250, 500, 750 and 1000 microM of vitamins K1 and K2, and 1, 10, 25, 50, 75 and 100 microM of vitamin K3 for 24 hours in an incubator atmosphere of 5% CO2, 37 degrees C and 100% humidity. Cell viability was estimated by MTT assay. Vitamin K1 showed no growth effect on all the glioma cells examined. Vitamin K2 did not cause any change in number of C6, however induced growth inhibition in a dose-dependent manner on glioblastoma multiforme. The IC50 values of vitamin K2 were 960 microM and 970 microM for glioblastoma multiforme, respectively. Vitamin K3 had also growth inhibitory effect in a dose-dependent manner on both C6 and glioblastoma multiforme. The IC50 values were 41 microM, 24 microM and 23 microM for vitamin K3, respectively. We concluded that vitamin K3 is more effective than vitamin K2 for inhibition of cancer cell growth, and might have an alternative value as an anticancer drug against glioblastoma multiforme.
16) http://www.ncbi.nlm.nih.gov/
Int J Mol Med. 2009 Jun;23(6):709-16.
Growth inhibitory effects of vitamin K2 on colon cancer cell lines via different types of cell death including autophagy and apoptosis. Kawakita H1, Tsuchida A, Miyazawa K, Naito M, Shigoka M, Kyo B, Enomoto M, Wada T, Katsumata K, Ohyashiki K, Itoh M, Tomoda A, Aoki T.
1Third Department of Surgery, Tokyo Medical University, Tokyo, Japan.
Vitamin K2 (menaquinone-4: MK4) has been reported to inhibit cell growth and induce apoptosis in various tumor cells. We examined the effects of MK4 using three types of colon cancer cell lines: PMCO1, COLO201, and DLD-1. Exposure to MK4 was at concentrations from 5 to 50 microM, growth inhibitory effects were observed dose-dependently in COLO201 and PMCO1, whereas the growth inhibition observed in DLD-1 was minimal. Comparison of COLO201 and PMCO1 cells exhibiting distinct growth inhibitory effects showed that cell death via apoptosis accompanied by activation of caspase-3 was induced in PMCO1, while apoptosis was not induced in COLO201. On the contrary, immunoblot assay using an anti-LC3B antibody showed autophagy induction by addition of MK4 and incubation in all three types of colon cancer cell lines. Addition of 3-methyladenine (3-MA) attenuated the growth inhibitory effect of MK4 in COLO201, whereas no influence of 3-MA was noted in PCMO1. Electron microscopy images of COLO201 showed that addition of MK4 induced an increased number of cytoplasmic autophagosomes and autolysosomes as well as morphological changes including scantiness of cytoplasm accompanied by loss of cell organelles, nuclear shrinkage, and fragmentation of cytoplasmic membrane in some cells, indicating the induction of cell death via autophagy not accompanied by the formation of apoptotic bodies in COLO201 cells. These results suggested that the response to MK4 and the way of induction of cell death vary in different colon cancer cell lines.
17) http://www.ncbi.nlm.nih.gov/
Int J Oncol. 2003 Sep;23(3):627-32.
Apoptosis induction of vitamin K2 in lung carcinoma cell lines: the possibility of vitamin K2 therapy for lung cancer. Yoshida T1, Miyazawa K, Kasuga I, Yokoyama T, Minemura K, Ustumi K, Aoshima M, Ohyashiki K. 1First Department of Internal Medicine, Tokyo Medical University, 6-7-1 Nishishinjuku, Shinjuku-ku, Tokyo 160-0023, Japan.
Vitamin K2 (menaquinone-4: VK2) has been reported to show apoptosis and differentiation-inducing effects on leukemia cells. Furthermore, the clinical benefits of using VK2 have been demonstrated for the treatment of the patients with acute leukemia and myelodysplastic syndromes. In the present study, we examined the in vitro effects of VK2 on lung carcinoma cell lines LU-139 and LU-130 for small cell carcinomas, PC-14 and CCL-185 for adenocarcinomas, LC-AI and LC-1/sq for squamous cell carcinomas, and IA-LM for large cell carcinoma, respectively. Treatment with VK2 for 48 to 96 h resulted in cell growth suppression in a dose-dependent manner in all cell lines tested. IC50 (50% inhibitory concentration) for VK2 ranged from 7.5 to 75 micro M, and there was no relation between the efficacy of growth suppression by VK2 and tissue type of lung carcinoma cell lines. Morphologic features of the cells treated with VK2 were typical for apoptosis along with caspase-3 activation and becoming positive for APO2.7 monoclonal antibody, an antibody which specifically detects the cell undergoing apoptosis. In addition to the leukemia cell line, LU-139 cells accumulated into G0/G1 phase during 72-h exposure to VK2. Combined treatment of cisplatin plus VK2 resulted in enhanced cytocidal effect compared to the cells treated with either cisplatin or VK2 alone. Since VK2 is a safe medicine without prominent adverse effects including bone marrow suppression, our data strongly suggest the therapeutic possibility of using VK2 for the treatment of patients with lung carcinoma.
18) http://www.ncbi.nlm.nih.gov/
J Gastroenterol Hepatol. 2010 Apr;25(4):738-44. doi: 10.1111/j.1440-1746.2009.
Available medical therapies against pancreatic cancer are largely ineffective and have many side-effects. Physiologically, vitamins K1 and K2 (VK) act as co-factors for gamma-carboxylation of prothrombin and other coagulation factors. In previous studies, VK analogs have been found to have potent negative effects on the survival of various cancer cells. We hypothesized that the well-tolerated and naturally occurring VK1 and VK2 may be used to inhibit pancreatic cancer cell survival.
METHODS:Four pancreas cancer cell lines were tested. Two of these (MiaPaCa2 and PL5) were found to be sensitive to VK1 and VK2 (IC50 values < or =150 microM). To address the mechanisms of this effect on cell survival, we performed cell cycle and apoptosis studies using VK2 (the more potent compound).
RESULTS:We found that VK induced caspase-dependent apoptosis in over 60% of cells in the sensitive lines at the half maximal inhibitory concentration (IC(50)) range. Further, this induction in apoptosis was antagonized by a caspase inhibitor. Accompanying apoptosis, a dose- and time-dependent induction of extracellular signal-regulated kinase (ERK) phosphorylation occurred when sensitive lines were treated with either VK1 or VK2 at inhibitory doses. Simultaneous co-treatment of cells with a MEK1 inhibitor and VK prevented both the induction of ERK phosphorylation and the apoptosis, showing that the mitogen-activated protein (MAP) kinase pathway is central for VK-mediated apoptosis in pancreatic cancer cells.
CONCLUSION:These data show that naturally-occurring, non-toxic K vitamins can inhibit the survival of some pancreatic cancer cell lines. These novel, safe and clinically-utilized agents initiate a caspase-dependent apoptosis via the MAP kinase pathway and could potentially benefit patients with pancreatic cancer either as a single agent or in combination with chemotherapy for treatment, or for prevention of recurrence of pancreas cancer post resection.
19) http://www.ncbi.nlm.nih.gov/
Int J Oncol. 2007 Aug;31(2):323-31.
Vitamins K2, K3 and K5 exert antitumor effects on established colorectal cancer in mice by inducing apoptotic death of tumor cells.
Ogawa M1, Nakai S, Deguchi A, Nonomura T, Masaki T, Uchida N, Yoshiji H, Kuriyama S.
Although a number of studies have shown that vitamin K possesses antitumor activities on various neoplastic cell lines, there are few reports demonstrating in vivo antitumor effects of vitamin K, and the antitumor effect on colorectal cancer (CRC) remains to be examined. Therefore, antitumor effects of vitamin K on CRC were examined both in vitro and in vivo. Vitamins K2, K3 and K5 suppressed the proliferation of colon 26 cells in a dose-dependent manner, while vitamin K1 did not. On flow cytometry, induction of apoptosis by vitamins K2, K3 and K5 was suggested by population in sub-G1 phase of the cell cycle. Hoechst 33342 staining and a two-color flow cytometric assay using fluorescein isothiocyanate-conjugated annexin V and propidium iodide confirmed that vitamins K2, K3 and K5 induced apoptotic death of colon 26 cells. Enzymatic activity of caspase-3 in colon 26 cells was significantly up-regulated by vitamins K2, K3 and K5. The pan-caspase inhibitor, benzyloxycarbonyl-Val-Ala-Asp-
20) http://www.ncbi.nlm.nih.gov/
Pharmazie. 2013 Jun;68(6):442-8.
Vitamin K4 induces tumor cytotoxicity in human prostate carcinoma PC-3 cells via the mitochondria-related apoptotic pathway.
Jiang Y1, Yang J, Yang C, Meng F, Zhou Y, Yu B, Khan M, Yang H.
1School of Life Sciences, Liaoning Provincial Key Laboratory of Biotechnology and Drug Discovery, Liaoning Normal University, Dalian, PR China.
vitamin K4 (VK4) is a synthetic hydrophilic menadione compound, which is clinically used as hemostasis medicine. It has been reported that several vitamin Ks had inhibitory effects on various cancer cells. However, there is no report about VK4s anticancer activity. The goal of this study was to investigate the inhibitory effect of VK4 on human prostate PC-3 cells and the mechanisms involved. We found that VK4 dose-dependently inhibited cell proliferation in PC-3 cells with an IC50 value of about 20.94 microM. Hoechst 33258 Staining results showed that VK4 caused DNA fragmentation in PC-3 cells. PI staining results indicated that VK4-induced PC-3 cell cycle arrest at the S phase. Further mechanistic studies revealed that VK4-mediated induction of apoptosis in PC-3 cell is associated with disruption of mitochondrial membrane potential, down-regulation of Bcl-2, and up-regulation of Bax, release of cytochrome c from mitochondria, and activation of caspase-3 and PARR Thus, VK4 might be useful in prostate cancer chemotherapy.
21) https://www.patrickholford.
Vitamin K: The Forgotten Vitamin Patrick Holford 2 Jul 2012
Vitamin K2 as a treatment for Rheumatoid Arthritis
22) http://www.ncbi.nlm.nih.gov/pubmed/18484089
IUBMB Life. 2008 Jun;60(6):355-61.
Vitamin K and rheumatoid arthritis. Okamoto H. Source Institute of Rheumatology, Tokyo Women’s Medical University, Tokyo, Japan.
Abstract Vitamin K2 [menaquinone-4 (MK-4)] has been reported to induce apoptosis in hepatocellular carcinoma, leukemia, and MDS cell lines. The effects of MK-4 on the development of arthritis have never been addressed so far. In this study, we investigated the effect of MK-4 upon the proliferation of rheumatoid synovial cells and the development of arthritis in collagen-induced arthritis (CIA). We analyzed the effect of MK-4 on the proliferation of fibroblast-like synoviocytes (FLSs) using the 3-(4,5-demethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay. The proapoptotic effect of MK-4 upon FLS was investigated with annexin V staining and DNA fragmentation and caspase 3/7 assays. Moreover, we analyzed the effect of MK-4 on the development of CIA in female dark agouti rats. Our results indicated that MK-4 inhibited the proliferation of FLS and the development of CIA in a dose-dependent manner. We concluded that MK-4 may represent a new agent for the treatment of RA in the setting of combination therapy with other disease-modifying antirheumatic drugs.
23) http://www.ncbi.nlm.nih.gov/
Int J Vitam Nutr Res. 1999 Jan;69(1):23-6.
Comparative effects of vitamin K2 and vitamin E on experimental arteriosclerosis.Seyama Y1, Hayashi M, Takegami H, Usami E.
1Department of Clinical Chemistry, Hoshi College of Pharmacy, Tokyo, Japan.
The comparative effects of vitamin K2 and vitamin E on aortic calcium (Ca) and inorganic phosphorus (P) levels in the aorta and the elastin fraction (fr.) were investigated in male rats after experimental arteriosclerosis was induced by vitamin D2 with atherogenic diet. Both vitamin K2 (100 mg/kg b.w.) and vitamin E (40 mg/kg b.w.) inhibited the increase of Ca and P in the aorta and the elastin fr. from the arteriosclerotic rats. Vitamin K2 (50 mg/kg b.w.) also suppressed the deposition of Ca and P in the aorta, but there was no change due to vitamin K3 or geranylgeraniol (side chain of vitamin K2) administration. Both vitamin K2 and vitamin E showed lipid radical scavenging activity in the in vitro experiment. However, neither vitamin K3 nor geranylgeraniol exhibited anti-arteriosclerotic or radical scavenging activity under the above experimental conditions. It is suggested that vitamin K2 and vitamin E promoted an antiarteriosclerotic effect by radical scavenging activity. These actions of vitamin K2 are required in the structure of 2-methylnaphtoquinone and its side chain (geranylgeraniol).
24)http://www.lmreview.com/articles/view/Vitamin-K2-Essential-for-Prevention-of-Age-Associated-Chronic-Disease/
Vitamin K2: Optimal Levels Essential for the Prevention of Age-Associated Chronic Disease by Lara Pizzorno, MDiv, MA, LMT
25)http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1915640/?report=classic
Osteoporos Int. Jul 2007; 18(7): 963–972.
Published online Feb 8, 2007.
Vitamin K2 supplementation improves hip bone geometry and bone strength indices in postmenopausal women
M. H. J. Knapen,2 L. J. Schurgers,1 and C. Vermeer corresponding author1,2,3 1VitaK, University of Maastricht, P.O. Box 616, 6200 MD Maastricht, The Netherlands 2CARIM, University of Maastricht, P.O. Box 616, 6200 MD Maastricht, The Netherlands
3Department of Biochemistry, University of Maastricht, P.O. Box 616, 6200 MD Maastricht, The Netherlands
26) http://www.ncbi.nlm.nih.gov/pubmed/17906277
Nutr Clin Pract. 2007 Oct;22(5):517-44.
Bone health and osteoporosis: the role of vitamin K and potential antagonism by anticoagulants. Pearson DA.
Vitamin K’s effects extend beyond blood clotting to include a role in bone metabolism and potential protection against osteoporosis. Vitamin K is required for the gamma-carboxylation of osteocalcin. Likewise, this gamma-carboxylation also occurs in the liver for several coagulation proteins. This mechanism is interrupted by coumarin-based anticoagulants in both the liver and bone.
METHODS: A thorough review of the literature on vitamin K, osteocalcin and their role in bone metabolism and osteoporosis, as well as the potential bone effects of anticoagulant therapy was conducted.
CONCLUSIONS: Epidemiological studies and clinical trials consistently indicate that vitamin K has a positive effect on bone mineral density and decreases fracture risk. Typical dietary intakes of vitamin K are below the levels associated with better BMD and reduced fracture risk; thus issues of increasing dietary intakes, supplementation, and/or fortification arise. To effectively address these issues, large-scale, intervention trials of vitamin K are needed. The effects of coumarin-based anticoagulants on bone health are more ambiguous, with retrospective studies suggesting that long-term therapy adversely affects vertebral BMD and fracture risk. Anticoagulants that do not affect vitamin K metabolism are now available and make clinical trials feasible to answer the question of whether coumarins adversely affect bone. The research suggests that at a minimum, clinicians should carefully assess anticoagulated patients for osteoporosis risk, monitor BMD, and refer them to dietitians for dietary and supplement advice on bone health. Further research is needed to make more efficacious decisions about vitamin K intake, anticoagulant therapy, and bone health.
Jeffrey Dach MD
7450 Griffin Road, Suite 190
Davie, Fl 33314
954-792-4663
http://www.jeffreydachmd.com
http://www.drdach.com
http://www.naturalmedicine101.com
Click Here for: Dr Dach’s Online Store for Pure Encapsulations Supplements
Click Here for: Dr Dach’s Online Store for Nature’s Sunshine Supplements
Web Site and Discussion Board Links:
http://jdach1.typepad.com/blog/
http://disc.yourwebapps.com/Indices/244124.html
http://disc.yourwebapps.com/Indices/244066.html
http://disc.yourwebapps.com/Indices/244067.html
http://disc.yourwebapps.com/Indices/244161.html
http://disc.yourwebapps.com/Indices/244163.html
Disclaimer click here: http://www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship. Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Copyright (c) 2014 Jeffrey Dach MD All Rights Reserved. This article may be reproduced on the internet without permission, provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.









Stuart A. Miller October 31, 2014 at 1:42 PM
F.Y.I., http://www.lef.org/magazine/2013/10/dr-l-ray-matthews-unleashes-the-power-of-vitamin-d/page-01
p j theut November 5, 2014 at 5:11 PM
k-vitamins.com
Cancer as a Metabolic Disease by Jeffrey Dach MD - Jeffrey Dach MD January 9, 2015 at 2:04 PM
[…] in blood coagulation, bone density, and prevention of soft tissue calcification. See my previous article on Vitamin K. Another surprising benefit of Vitamin K is cancer prevention. A number of cell […]