Natural Thyroid is Better Part Two by Jeffrey Dach MD
This article is part two of a series. For Part One, Click Here. For Part Three Click here.
Will Thyroid Medication Give Me Osteoporosis ?
New concerns were raised by Marci Turner in the April 2011 British Medical Journal reporting elderly women on Synthroid(tm) have increased fracture risk.(13)
A previous 2010 report by Murphy looked at thyroid function and fracture risk in normal postmenopausal women, and they found a 35% increase in fracture risk in women with lower TSH values (TSH=thyroid stimulating hormone). (1) Higher TSH was protective of fracture.
No Real Consensus on The Issue
To add confusion, a 2003 meta-analysis by Schneider reviewed 63 studies looking at the effect of thyroid medication (T4-only) on bone mineral density, finding no real concensus and concluding that, “currently debate still exists about the effects of thyroid hormone therapy on skeletal integrity, that is the safety of levothyroxine use with respect to bone mineral density.” (14)(15)
Let’s take a look at this issue and try to come up with some real answers.
The Calcitonin Connection
 The thyroid gland not only makes thyroid hormone. It also makes Calcitonin, a hormone manufactured by the parafollicular calls (C cells) in the thyroid tissue. Calcitonin is involved in calcium metabolism, bone maintenance and prevents osteoporosis.
The thyroid gland not only makes thyroid hormone. It also makes Calcitonin, a hormone manufactured by the parafollicular calls (C cells) in the thyroid tissue. Calcitonin is involved in calcium metabolism, bone maintenance and prevents osteoporosis.
Left image: Calcitonin courtesy of wikimedia commons
Thyroid disorders cause destruction of calcitonin cells
Hashimoto’s thyroiditis is a common cause of hypothyroidism and is associated with destruction of the C-cells and loss of calcitonin production. (2-4) The resulting Calcitonin deficiency is a potential cause of bone resorption and osteoporosis. (7-12)
Hashimoto’s, radio-iodine and surgery all destroy Calcitonin Cells
The autoimmune process of Hashimotos’, thyroid ablation with radioactive iodine and/or surgery all reduce or eliminate thyroid function, and the C-cells which make calcitonin may be destroyed or reduced in number as well.
Synthroid, levothyroxine, and T4-only medications do not provide the missing calcitonin. One would expect the calcitonin deficient patient to be at greater risk for osteoporosis and fracture. Unlike Synthroid and T4-only medications which DO NOT contain calcitonin, natural desiccated thyroid DOES CONTAIN calcitonin, providing the missing hormone, and is the preferred form of thyroid medication.
None of the Studies Used Natural Desiccated Thyroid
 Unfortunately. all of the medical studies that examined the bone-thyroid connection used T4-only medication, none used desiccated natural thyroid, so we don’t have a good comparison study to evaluate the long term lack of osteoporosis from natural desiccated thyroid. A good use of NIH research funding would be comparing the bone density and long term risk of fracture with natural desiccated thyroid compared to T4 only medications. Don’t hold your breathe. The NIH is a government agency, and the government is influenced by Big Pharma dollars, so natural is out and synthetic is in. We may never see NIH funding for natural desiccated thyroid.
Unfortunately. all of the medical studies that examined the bone-thyroid connection used T4-only medication, none used desiccated natural thyroid, so we don’t have a good comparison study to evaluate the long term lack of osteoporosis from natural desiccated thyroid. A good use of NIH research funding would be comparing the bone density and long term risk of fracture with natural desiccated thyroid compared to T4 only medications. Don’t hold your breathe. The NIH is a government agency, and the government is influenced by Big Pharma dollars, so natural is out and synthetic is in. We may never see NIH funding for natural desiccated thyroid.
Above Left image: chemical structure of thyroxine, T4 courtesy of wikimedia commons
The TSH Connection. TSH is Protective and Prevents Bone Resorption
Advances in our understanding of physiology and animal research have revealed TSH hormone (thyroid stimulating hormone) has a direct effect on bone cells, preventing degradation of bone and bone resorption, and therefore protective of bone density.(17-19) This could explain the many studies that find a correlation between higher TSH and improved bone density. The problem with using TSH as a treatment for osteoporosis is that higher TSH is associated with increased heart disease (see the HUNT study), as well as a host of low thyroid symptoms of fatigue, malaise, muscle aches and pains etc. Patients feel better with a lower TSH and higher thyroid function, so cutting back on thyroid medication to let the TSH drift up may be good for bone density, but it is not good for the patient.
Good News About Bioidentical Hormones
The good news is that the TSH effect on bone density is relatively modest and is offset by the addition of estrogen, a bioidentical hormone, which increases bone density. (20) In addition, we routinely employ a natural bone building program to optimize vitamin D levels which protects and maintains bone density.
In conclusion, an excellent reason to switch from T4-only thyroid medication to natural desiccated thyroid is because it contains Calcitonin, protective of bone density and preventive of osteoporosis. T4-only medication does not contain calcitonin and is associated with loss of bone density and increased fracture risk. We have found good clinical results with a natural dessicated thyroid product called Naturethroid from RLC labs. Dosage range is from one to four Grains per day depending on underlying thyroid function and body weight.
Atricles with Related Interest : This is Part Two of the article.
For Part One of this article, click here
For Part Three, Click here.
Selenium and Thyroid More Good News
New Study shows Natural Thyroid Better than Synthroid
Why Natural Thyroid is Better than Synthetic Part One
Why Natural Thyroid is Better Part Two
The TSH Reference Range Wars – Part One
Jeffrey Dach MD
7450 Griffin Road
Davie, Fl 33314
954-983-1443
Other Books Also Recommended:
Hypothyroidism the Unsuspected Illness, by Broda Barnes MD
Iodine, Why You Need It and Why You Cant Live Without It by David Brownstein MD
Hypothyroidism, Type Two by Mark Starr MD
Adrenal Fatigue: The 21st Century Stress Syndrome by Wilson
jeffrey dach md
Links and Refernences
(1) http://www.ncbi.nlm.nih.gov/pubmed/20410228
J Clin Endocrinol Metab. 2010 Jul;95(7):3173-81. Epub 2010 Apr 21.
Thyroid function within the upper normal range is associated with reduced bone mineral density and an increased risk of nonvertebral fractures in healthy euthyroid postmenopausal women. Murphy E, Glüer CC, Reid DM, Felsenberg D, Roux C, Eastell R, Williams GR. Molecular Endocrinology Group, 7th Floor Commonwealth Building, Hammersmith Hospital, Du Cane Road, London W12 0NN, United Kingdom.
CONTEXT: The relationship between thyroid function and bone mineral density (BMD) is controversial. Existing studies are conflicting and confounded by differences in study design, small patient numbers, and sparse prospective data. OBJECTIVE: We hypothesized that variation across the normal range of thyroid status in healthy postmenopausal women is associated with differences in BMD and fracture susceptibility.
DESIGN: The Osteoporosis and Ultrasound Study (OPUS) is a 6-yr prospective study of fracture-related factors. SETTING: We studied a population-based cohort from five European cities.
PARTICIPANTS: A total of 2374 postmenopausal women participated. Subjects with thyroid disease and nonthyroidal illness and those receiving drugs affecting thyroid status or bone metabolism were excluded, leaving a study population of 1278 healthy euthyroid postmenopausal women. INTERVENTIONS: There were no interventions. MAIN OUTCOME MEASURES: We measured free T(4) (fT4) (picomoles/liter), free T(3) (fT3) (picomoles/liter), TSH (milliunits/liter), bone turnover markers, BMD, and vertebral, hip, and nonvertebral fractures.
RESULTS: Higher fT4 (beta = -0.091; P = 0.004) and fT3 (beta = -0.087; P = 0.005) were associated with lower BMD at the hip, and higher fT4 was associated with increasing bone loss at the hip (beta = -0.09; P = 0.015). After adjustment for age, body mass index, and BMD, the risk of nonvertebral fracture was increased by 20% (P = 0.002) and 33% (P = 0.006) in women with higher fT4 or fT3, respectively, whereas higher TSH was protective and the risk was reduced by 35% (P = 0.028). There were independent associations between fT3 and pulse rate (beta = 0.080; P = 0.006), increased grip strength (beta = 0.171; P<0.001), and better balance (beta = 0.099; P < 0.001), indicating that the relationship between thyroid status and fracture risk is complex.
CONCLUSIONS: Physiological variation in normal thyroid status is related to BMD and nonvertebral fracture.
————————————————–
Hashimoto’s destroys the C-cells (calcitonin) cells
(2) http://www.ncbi.nlm.nih.gov/pubmed/9669288
Thyroid. 1998 Jun;8(6):505-9. Quantitative analysis of C cells in Hashimoto’s thyroiditis.
Lima MA, Santos BM, Borges MF. Brazil.
The objective of the present investigation was to study quantitatively C cells in Hashimoto’s thyroiditis (HT) by analyzing 22 thyroids obtained at autopsy or thyroidectomy from 16 patients with thyroiditis and from 6 normal subjects. Six different areas were sampled on average and labeled with a monoclonal anticalcitonin antibody by immunohistochemistry using the avidin-biotin-peroxidase complex. Normal thyroids from adult patients with no thyroid disease were used as control. C cells were counted in 1 cm2 fields and the mean number of cells per field was calculated. Data were analyzed statistically by the Mann-Whitney test. The inflammatory process detected in cases of HT was usually moderate (50%) and the number of C cells ranged from 0 to 12.2 per 1 cm2 field. The number of C cells in normal thyroids ranged from 20 to 148 per 1 cm2 field, with a median of 35.2 cells per field. The results demonstrate a significant decrease in C cell number in HT compared with normal thyroids, indicating that the inflammatory process causes destruction of both follicular and C cells, which are replaced by fibrosis.
(3) http://www.ncbi.nlm.nih.gov/pubmed/9797849
Calcitonin deficiency in early stages of chronic autoimmune thyroiditis
Borges MF, Abelin NM, Menezes FO, Dahia PL, Toledo SP. Department of Medicine, Federal School of Medicine of Triângulo Mineiro, Uberaba, Brazil.
OBJECTIVES: Although calcitonin (Ct) deficiency has been described in chronic autoimmune thyroiditis (CAT) it is unclear at what stage in the disease it develops. We have analysed the Ct secretory responses of patients in two different evolutionary stages of CAT, namely the goitrous and atrophic phases. DESIGN: We studied the Ct response to combined calcium (2 mg/kg) and pentagastrin (0.5 microgram/kg) intravenous infusion in 27 patients with CAT and 30 normal adult controls. The cases were divided into two groups. The first comprised eleven women with CAT and goitrous subclinical hypothyroidism (GH), aged 28.6 +/- 10.1 years–at diagnosis they had increased thyroid autoantibody titres and cytological features compatible with stages 1 and 2 of Hashimoto’s thyroiditis. The second comprised 16 females with CAT and an atrophic thyroid confirmed by ultrasound scan, aged 38.0 +/- 9.2 years–these patients were severely hypothyroid at diagnosis and were termed AH (atrophic hypothyroidism). Both groups (GH and AH) received replacement doses of thyroxine sufficient to restore euthyroidism for at least six months before the stimulation tests. Control group (C) consisted of 20 healthy women (A), aged 30.0 +/- 9.6 years, and 10 healthy men (, aged 34.7 +/- 8.0 years. Serum Ct was measured by IRMA. The Ct secretory response was related to thyroid size and cytological data, when available. RESULTS: Basal Ct concentrations in groups GH (0.08 ng/l, median) and AH (0.07 ng/l, median) were significantly lower than those of female controls (0.58 ng/l, median). Stimulated Ct peak values in groups GH (0.08 ng/l, median) and AH (0.19 ng/l, median) were significantly lower than those of female controls (13.61 ng/l, median). Also, both basal (2.72 ng/l, median) and stimulated Ct levels (35.73 ng/l, median) in male controls were significantly higher than in female controls given already. A positive correlation between the Ct secretory reserve and thyroid dimensions, evaluated by ultrasound scan, was found only in patients with thyroid atrophy (AH; rs = 0.61, P < 0.05). CONCLUSIONS: We have found low basal and stimulated calcitonin values in patients with chronic autoimmune thyroiditis and thyroid enlargement, which represents an early phase of chronic autoimmune thyroiditis. Our data have also confirmed previous findings of deficient calcitonin secretion in advanced stages of chronic autoimmune thyroiditis in which thyroid atrophy is usually found. These findings may be associated with C-cell destruction following progressive, nonspecific follicular cell damage caused by lymphocytic infiltration and fibrosis of the gland.
(4) http://www.ncbi.nlm.nih.gov/pubmed/10646660
Thyroid. 1999 Dec;9(12):1211-4. Calcitonin reserve in different stages of atrophic autoimmune thyroiditis. Poppe K, Verbruggen LA, Velkeniers B, Finné E, Body JJ, Vanhaelst L.
The objective of this study was to determine the calcitonin (CT) hormone reserve in different severity of atrophic autoimmune thyroiditis (AAT). Forty-eight female patients with AAT were divided into four groups based on basal and peak thyrotropin (TSH) values (after oral thyrotropin-releasing hormone [TRH], free triiodothyronine (FT3) and free thyroxine (FT4) ranging from normal in group 1 to overt hypothyroidism in group 4.
All had thyroid antibodies. The control group comprised euthyroid females of comparable age, without thyroid antibodies. Basal CT and CT response to calcium infusion (area under the curve) were investigated as parameters of CT reserve. Basal CT was lower in groups 2 to 4 of patients with AAT (compared to controls), but the difference was not significant. Stimulated CT levels were lower (p < 0.05) in all groups of patients compared to controls, with markedly reduced CT-secretory reserve in group 4. Thyroid antibody concentrations and, basal and postinfusion calcium levels were not significantly different among the various groups.
In conclusion CT deficiency (especially stimulated values) occurs in AAT and is more severe in hypothyroid patients than in earlier stages of AAT.
=============================================
Prophylactic Treatment of Hashimotos with Normal Thyroid Labs is Beneficial, reduces lymphocyte infiltration and antibody levels.
(5) http://www.ncbi.nlm.nih.gov/pubmed/11327616
Thyroid. 2001 Mar;11(3):249-55. One-year prophylactic treatment of euthyroid Hashimoto’s thyroiditis patients with levothyroxine: is there a benefit? Padberg S, Heller K, Usadel KH, Schumm-Draeger PM. SourceMedica Clinic l, Endocrinology, Center of Internal Medicine, Johann Wolfgang Goethe-University, Frankfurt/Main, Germany.
Studies in animal models of spontaneous Hashimoto’s autoimmune thyroiditis (HT) show that prophylactic treatment with levothyroxine (LT4) can reduce incidence and degree of lymphocytic infiltration in HT. The aim of the present study was to clarify whether there is a benefit of prophylactic treatment with LT4 in patients with euthyroid HT with respect to the progression of the autoimmune process. Twenty-one patients with euthyroid HT were checked for thyroid function (thyrotropin [TSH], free triiodothyronine [FT3], free thyroxine [FT4]), thyroid volume, antibodies (thyroglobulin [Tg-Ab], thyroid peroxidase [TPO-Ab]), and lymphocyte subsets. Peripheral (PBL) and thyroid-derived lymphocytes (TL) were analyzed by triple color flow cytometry.
One-half of the patients with euthyroid HT were treated with LT4 for 1 year (n = 10). The other half (n = 11) were never treated with LT4. TL were obtained by fine-needle aspiration biopsy (FNA![]() . Thirteen healthy subjects (C) without medical history of thyroid disease served as controls concerning PBL, and patients with non-toxic nodular goiter (NG; n = 10) served as controls concerning TL. Thyroid-derived T-helper cells were found more frequently in euthyroid patients with HT compared to patients with NG (p < 0.01).
. Thirteen healthy subjects (C) without medical history of thyroid disease served as controls concerning PBL, and patients with non-toxic nodular goiter (NG; n = 10) served as controls concerning TL. Thyroid-derived T-helper cells were found more frequently in euthyroid patients with HT compared to patients with NG (p < 0.01).
After 1 year of therapy with LT4, TPO-Abs and B lymphocytes decreased significantly only in the treated group of euthyroid patients with HT (p < 0.05). In contrast, TPO-Abs levels did not change or even increased in untreated euthyroid patients with HT. Thyroid volume did not differ before and after therapy.
Prophylactic treatment of euthyroid patients with HT reduced both serological and cellular markers of autoimmune thyroiditis. Therefore, prophylactic LT4 treatment might be useful to stop the progression or even manifestation of the disease. However, the long-term clinical benefit of prophylactic LT4 therapy in euthyroid patients with HT is yet to be established.
(6) http://www.ncbi.nlm.nih.gov/pubmed/16006728
Endocr J. 2005 Jun;52(3):337-43. Effects of prophylactic thyroid hormone replacement in euthyroid Hashimoto’s thyroiditis. Aksoy DY, Kerimoglu U, Okur H, Canpinar H, Karaagaoglu E, Yetgin S, Kansu E, Gedik O. Source Section of Endocrinology and Metabolism, Department of Internal Medicine, Hacettepe University, Ankara, Turkey.
Abstract
Hashimoto’s thyroiditis is the most frequent autoimmune thyroid disease. L-thyroxine therapy can reduce the incidence and alleviate the symptoms of this disease. The aim of this study was to evaluate the effects of prophylactic L-thyroxine treatment on clinical and laboratory findings of patients who were euthyroid at the time of diagnosis. Thirty-three patients who had diagnosis of euthyroid Hashimoto’s thyroiditis were randomized to two groups, one group received prophylactic L-thyroxine treatment and the other was followed-up without treatment. Initial thyroid function tests, autoantibodies, ultrasonography, fine needle aspiration biopsy and peripheral blood lymphocyte subsets were similar in the two study groups. After 15 months of L-thyroxine treatment, there was a significant increase in free T4 and a significant decrease in TSH and anti-thyroglobulin antibody anti-thyroid peroxidase antibody levels. CD8+ cell counts increased in both groups, CD4/CD8 levels decreased significantly because of the increase in CD8+ cell count levels. Though there was no change in cytological findings, ultrasonography showed a decrease in thyroid volume in L-thyroxine receiving patients whereas an increase was detected in patients who were followed without treatment. In conclusion, prophylactic thyroid hormone therapy can be used in patients with Hashimoto’s thyroiditis even if they are euthyroid.
Calcitonin
(7) http://endo.endojournals.org/cgi/content/full/147/9/4007
Endocrinology Vol. 147, No. 9 4007-4009
Calcitonin—Guardian of the Mammalian Skeleton or Is It Just a Fish Story? Scott Miller
(8) http://endo.endojournals.org/cgi/content/abstract/147/9/4010?ijkey=bd61473312d62e7a5ef50cedc6ef1baa19c21cf3&keytype2=tf_ipsecsha
Endocrinology Vol. 147, No. 9 4010-4021
Calcitonin Plays a Critical Role in Regulating Skeletal Mineral Metabolism during Lactation. Janine P. Woodrow, Christopher J. Sharpe, Neva J. Fudge, Ana O. Hoff, Robert F. Gagel and Christopher S. Kovacs
The maternal skeleton rapidly demineralizes during lactation to provide calcium to milk, responding to the stimuli of estrogen deficiency and mammary-secreted PTH-related protein. We used calcitonin/calcitonin gene-related peptide- (Ctcgrp) null mice to determine whether calcitonin also modulates lactational mineral metabolism. During 21 d of lactation, spine bone mineral content dropped 53.6% in Ctcgrp nulls vs. 23.6% in wild-type (WT) siblings (P < 0.0002). After weaning, bone mineral content returned fully to baseline in 18.1 d in Ctcgrp null vs. 13.1 d in WT (P < 0.01) mice. Daily treatment with salmon calcitonin from the onset of lactation normalized the losses in Ctcgrp null mice, whereas calcitonin gene-related peptide- or vehicle was without effect. Compared with WT, Ctcgrp null mice had increased circulating levels of PTH and up-regulation of mammary gland PTH-related protein mRNA. In addition, lactation caused the Ctcgrp null skeleton to undergo more trabecular thinning and increased trabecular separation compared with WT. Our studies confirm that an important physiological role of calcitonin is to protect the maternal skeleton against excessive resorption and attendant fragility during lactation and reveal that the postweaning skeleton has the remarkable ability to rapidly recover even from losses of over 50% of skeletal mineral content.
(9) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2680171/
J Bone Miner Res. 2008 August; 23(8): 1182–1193. Calcitonin Receptor Plays a Physiological Role to Protect Against Hypercalcemia in Mice
Rachel A Davey,1 Andrew G Turner,1 Julie F McManus,1 WS Maria Chiu,1 Francisca Tjahyono,1 Alison J Moore,2 Gerald J Atkins,2,3 Paul H Anderson,2 Cathy Ma,1 Vaida Glatt,4 Helen E MacLean,1 Cristina Vincent,2 Mary Bouxsein,4 Howard A Morris,2 David M Findlay,2,3 and Jeffrey D Zajac1
Whereas it is well established that calcitonin potently inhibits bone resorption through the interaction with the CTR on osteoclasts in vitro, the physiological role of calcitonin remains an area of debate.
Post-Thyroidectomy, Calcitonin and Osteoporosis
(10) http://www.ncbi.nlm.nih.gov/pubmed/10230474
Acta Med Austriaca. 1999;26(1):29-31. Possible effect of calcitonin deficiency on bone mass after subtotal thyroidectomy. Mirzaei S, Krotla G, Knoll P, Koriska K, Köhn H.
SourceDepartment of Nuclear Medicine, Wilhelminenspital, Vienna, Austria.
Abstract
Bone mass is purportedly reduced by an excess of endogenous or exogenous thyroid hormone or perhaps by calcitonin deficiency. Patients who have undergone thyroidectomy could be subject to all of these effects. In the present study we tried to demonstrate, whether lack of calcitonin following thyroidectomy has a significant influence on bone density. We measured thyroid hormone levels, TSH and calcitonin and assessed the bone mass in the hip and lumbar spine of 55 patients (32 f, 23 m), who had undergone a subtotal thyroidectomy between 1938 and 1996 on the reason of a non-toxic goitre. TSH levels were suppressed in 16 patients. Serum concentration of total calcium, intact PTH, osteocalcin were normal in all subjects. The mean fasting calcitonin level was in the patient group 2.09 +/- 0.7 pg/ml and in the control group, age matched healthy volunteers, 2.8 +/- 1.2 pg/ml. However, the serum level of calcitonin was not significantly lower than in the control group. 43 patients had an osteopenia or osteoporosis. The interpretation of the results in this study is hampered by the fact, that in women results may be influenced by involutional osteoporosis. Therefore we focus on the potential for osteoporosis among the 23 men. The results of our study indicates, that there is a significant reduction in bone mass in male after thyroidectomy, no matter whether T4 therapy is given or not, and whether TSH is suppressed or in a normal range.
(11) Minerva Endocrinol. 2004 Mar;29(1):1-10.
[Bone density and mineral metabolism in calcitonin-deficiency patients].
AIM: Calcitonin is a hormone secreted by thyroid C-cells. Its primary effect seems to be a direct inhibition of bone degradation, but the physiological function of calcitonin in humans is still uncertain. The role of this hormone in the development of osteoporosis is unknown, but few authors have shown bone mass reduction in thyroidectomy patients.
METHODS: To investigate the influence of calcitonin deficiency on bone turnover, 9 males (age 31 to 66 years) submitted to total thyroidectomy in 1996 for non-toxic goitre have been studied. These patients received thyroxine treatment at individual dose but never with suppressed TSH levels. Moreover 8 sex-, age- and Body Mass Index-matched normal subjects have also been studied as control group.
RESULTS: Calcitonin was undetectable in thyroidectomized patients, while the mean value was 7.1+/-3.2 pg/ml in the control group. At bone ultrasonography 50% of patients showed osteopenia, while only 1 subject showed osteopenia in the control group. The mean calcium serum level of patients was significant lower than in the control group (p<0.001). Calcium urinary level was increased in patients than controls. PTH serum levels were statistically decreased (p<0.001) in patients more than in controls. Osteocalcin showed a significantly (p<0.05) lower bone formation in patients than in controls, while the markers of resorption, deoxypyridinoline and N-terminal telopeptide of type I collagen, suggested an increased bone turnover in calcitonin-deficiency patients.
CONCLUSION: The results of this study show that the chronic lack of calcitonin in total thyroidectomized patients may play a role in increased bone degradation and osteopenia with a higher risk of bone fracture.
(12) http://www.ncbi.nlm.nih.gov/pubmed/1929193
Ann Endocrinol (Paris). 1991;52(2):109-12. [Chronic autoimmune thyroiditis and C-cell hyperplasia. Study of calcitonin secretion in 24 patients].[Article in French]Barbot N, Guyetant S, Beldent V, Akrass A, Cerf I, Perdrisot R, Bigorgne JC.
Serum calcitonin (CT) was determined by radioimmunoassay, using two monoclonal antisera, in 22 women and two men, who had Hashimoto’s thyroiditis as confirmed by echographic, immunological or cytological criteria; in 23 patients, serum CT levels were measured after intravenous infusion of pentagastrin (Pg). In 21 cases, basal and Pg stimulated serum CT concentrations were normal. A 61-year-old woman and a 63-year-old man, both euthyroid, had high serum basal CT: 12 pg/ml and 35 pg/ml; infusion of Pg resulted in abnormal increases in serum CT levels: respectively 64 pg/ml and 115 pg/ml. Another patient, a 65-year-old woman with primary hypothyroidism had high serum basal CT: 90 pg/ml (the Pg stimulation test was not done because of ischemic heart disease). Each of these 3 patients had a total thyroidectomy. Pathological examination of the thyroid showed typical features of Hashimoto’s thyroiditis and extensive C-cell hyperplasia. After surgery, serum CT levels fell to normal. Therefore, a high serum CT can be observed as the consequence of C-cell hyperplasia in Hashimoto’s thyroiditis.
———————–
Older patients on Thyroxine have increased fracture risk- they did not look at thyroid function, TSH, Abs etc. Are these pats hashimotos with Calcitonin loss?
(13) http://www.bmj.com/content/342/bmj.d2238.full
BMJ 2011; 342:d2238 Levothyroxine dose and risk of fractures in older adults: nested case-control study. Marci R Turner, medical resident1, Ximena Camacho, analyst2, Hadas D Fischer, epidemiologist2, Peter C Austin, senior scientist2, Geoff M Anderson, professor3, Paula A Rochon, senior scientist4, Lorraine L Lipscombe, scientist4
Design Nested case-control study.
Setting Population based health databases, Ontario, Canada.
Participants Adults aged 70 or more prescribed levothyroxine between 1 April 2002 and 31 March 2007 and followed for fractures until 31 March 2008. Cases were cohort members admitted to hospital for any fracture, matched with up to five controls from within the cohort who had not yet had a fracture.
Main outcome measure Primary outcome was fracture (wrist or forearm, shoulder or upper arm, thoracic spine, lumbar spine and pelvis, hip or femur, or lower leg or ankle) in relation to levothyroxine use (current, recent past, remote). Risk among current users was compared between those prescribed high, medium, and low cumulative levothyroxine doses in the year before fracture.
Results Of 213 511 prevalent levothyroxine users identified, 22 236 (10.4%) experienced a fracture over a mean 3.8 years of follow-up, 18 108 (88%) of whom were women. Compared with remote levothyroxine use, current use was associated with a significantly higher risk of fracture (adjusted odds ratio 1.88, 95% confidence interval 1.71 to 2.05), despite adjustment for numerous risk factors. Among current users, high and medium cumulative doses (>0.093 mg/day and 0.044-0.093 mg/day) were associated with a significantly increased risk of fracture compared with low cumulative doses (<0.044 mg/day): 3.45 (3.27 to 3.65) and 2.62 (2.50 to 2.76), respectively.
Conclusion Among adults aged 70 or more, current levothyroxine treatment was associated with a significantly increased risk of fracture, with a strong dose-response relation. Ongoing monitoring of levothyroxine dose is important to avoid overtreatment in this population.
Our findings provide evidence that levothyroxine treatment may increase the risk of fragility fractures in older people even at conventional dosages, suggesting that closer monitoring and modification of treatment targets may be warranted in this vulnerable population.
Thyroid hormone and Bone Density-
Clinical Review of 63 studies – Mixed results- No proven effects
(14) http://www.ncbi.nlm.nih.gov/pubmed/14714266
Exp Clin Endocrinol Diabetes. 2003 Dec;111(8):455-70. The effect of levothyroxine therapy on bone mineral density: a systematic review of the literature. Schneider R, Reiners C. Source Clinic for Nuclear Medicine, University of Würzburg, Germany.
BACKGROUND: Currently debate still exists about the effects of thyroid hormone therapy on skeletal integrity, that is the safety of levothyroxine use with respect to bone mineral density.
OBJECTIVE: A systematic review of the effects of TSH-suppressive and replacement levothyroxine therapy on bone mineral density evaluated main causes of conflicting results and its implications for clinical practice, and suggested directions of future research. DATA SOURCE AND STUDY SELECTION: A MEDLINE search identified English-language studies assessing bone mineral density under levothyroxine therapy published from 1990 to 2001.
DATA EXTRACTION: The studies were grouped by design and type of intervention. Outcomes were qualitatively analysed. Subgroup analysis assessed heterogeneity between studies.
DATA SYNTHESIS: Of 63 identified studies, 31 studies reported no effects of levothyroxine on bone mineral density, 23 studies showed partial beneficial or adverse, and 9 studies overall adverse effects. A significant dose-response was not found. There was a tendency towards peripheral cortical bone loss, suggesting a site-specific effect. In adolescents, men, and premenopausal women evidence for levothyroxine influence was weaker than in postmenopausal women. However, also findings in postmenopausal women remained unclear. The extent and etiology of underlying thyroid diseases also contributed to inconsistent results. Further, controversial results were due to substantial heterogeneity of studies. Above all, studies were limited by moderate quality, small size, and inadequate control for confounders.
CONCLUSIONS: Based on current studies there is insufficient evidence about effectiveness of levothyroxine on bone mineral density. All conclusions, however, must take into account the important methodical drawbacks. Present data may only be proved by longitudinal, high quality studies in homogeneous patients with sufficient sample size, clinical implication of future research remains questionable, though.
(15) http://thyroid.about.com/cs/osteoporosis/a/osteoporosis_2.htm
Is Thyroid Medication Going to Give You Osteoporosis? Experts Evaluate the Risks
What Does this Mean for Patients? From Mary J. Shomon and Dr. William Cline March 11, 2004
NASAL Calcitonion in Men with Osteoporosis – increases bone density
(16) http://www.ncbi.nlm.nih.gov/pubmed/11874243
J Bone Miner Res. 2002 Mar;17(3):521-7.
A randomized trial of nasal spray salmon calcitonin in men with idiopathic osteoporosis: effects on bone mineral density and bone markers. Trovas GP, Lyritis GP, Galanos A, Raptou P, Constantelou E. SourceLaboratory for the Research of Musculoskeletal System, University of Athens, Greece.
Abstract
In a 12-month randomized, double-blind, placebo-controlled trial, we have studied the effects of intranasal salmon calcitonin (SCT) on bone mineral density (BMD) and biochemical markers of bone turnover. Twenty-eight men with idiopathic osteoporosis aged 27-74 years (mean, 52.4 years) were randomized to receive either nasal SCT (200 IU) or a nasal placebo daily for a period of 1 year. All the men received a daily supplement of 0.5 g of calcium. The men who received SCT had a mean (+/-SEM) increase in BMD of 7.1 +/- 1.7% at the lumbar spine. In contrast, the men who received the placebo had an increase of 2.4 +/- 1.5% (p > 0.05) for the comparison with baseline. The increase in lumbar BMD in the calcitonin group was significantly greater than that in the placebo group (p < 0.05). There were no significant changes in the femoral neck, trochanter, or Ward’s triangle relative to both baseline and placebo after 12 months. Treatment with nasal SCT resulted in a significantly pronounced suppression of bone resorption markers (urinary deoxypyridinoline [DPD], type I cross-linked N-telopeptide [NTX], and type I cross-linked C-telopeptide [CTX]) and to a lesser extent in bone formation markers (serum bone-specific alkaline phosphatase [BALP], osteocalcin [OC], serum C-terminal procollagen type I extension peptides [PICP], and serum N-termnal procollagen type I extension peptides [PINP]), whereas the placebo did not. Therapy was tolerated well and there were no treatment-related adverse events.
We conclude that intranasal SCT (200 IU daily) is safe and effective in increasing lumbar BMD and reducing bone turnover in men with idiopathic osteoporosis.
TSH itself plays a role in increasing bone density
(17) http://www.ncbi.nlm.nih.gov/pubmed/20151763
Endocr Regul. 2010 Jan;44(1):9-15.
The level of TSH appeared favourable in maintaining bone mineral density in postmenopausal women. Baqi L, Payer J, Killinger Z, Susienkova K, Jackuliak P, Cierny D, Langer P. Source5th Clinic of Internal Medicine, Faculty Hospital Ruzinov, and Department of Statistics, Economics University, Bratislava, Slovakia.
Abstract
OBJECTIVE: Since the positive role of thyrotropin (TSH) in bone remodeling has been recently emphasized, this cross-section study is aimed to evaluate the association of bone status with the level of TSH and free thyroxine (FT4) in the cohort of postmenopausal women after long-term treatment of thyroid disorders and age matched controls.
METHODS: Urinary calcium (dUCa) and serum level of TSH, FT4 and of bone turnover markers (BTMs) such as alkaline phosphatase (ALP), osteocalcin (OC), cross linked N-telopeptide of type 1 collagen (NTx) as well as lumbar spine L 1-4 (BMD-L) and femoral hip (BMD-F) mineral density were determined in 113 postmenopausal women consisting of 42 patients with Graves disease treated by carbimazole, 32 patients with thyroid cancer treated with L-thyroxine and 39 age matched women without any thyroid and osteological disorders. For statistical evaluation t-test, Pearson’s correlation coefficient and linear multiple regression were used.
RESULTS: To compare the association of TSH versus FT4 with BMD and BTMs the pooled cohort of all 113 women was divided in two groups in terms of TSH level:
1. 34 women with low TSH (below 0.50 mU/l);
2. 79 women with normal TSH (0.51-4.3 mU/l).
In spite of significantly higher FT4 level, the Group 2 with normal TSH level had significantly higher BMD-L and BMD-F (p<0.001) and, in contrast, significantly lower urinary dUCa, ALP, OC (all at p<0.001) and NTx (p<0.01) as compared to the Group 1 with low TSH level. Linear multiple regression showed highly significant influence of TSH on BMD-L and BMD-F0 (p<0.001) independent of age, FT4 and body mass index, while that of FT4 was not significant. The strength of linear interrelation between all variables used was finally tested by Pearson’s correlation coefficient (Table 3) which was highly positive for TSH with BMD-F and BMD-L, but highly negative for TSH with serum NTx, OC, ALP) and urinary calcium (dUCa). In contrast, no significant correlation was found between the level of FT4 and BMD.
CONCLUSIONS: Irrespectively of FT4 level, postmenopausal women with normal TSH level showed a favorable bone status as compared to these with low level of TSH which is consistent with the view that TSH itself possibly participates in playing a favorable role in influencing the bone mineral density in adult women.
TSH has direct effect on bone by inhibiting bone resorption
(18) http://www.ncbi.nlm.nih.gov/pubmed/15746993
J Bone Miner Res. 2005 Mar;20(3):480-6. Epub 2004 Nov 29.
Recombinant human TSH modulates in vivo C-telopeptides of type-1 collagen and bone alkaline phosphatase, but not osteoprotegerin production in postmenopausal women monitored for differentiated thyroid carcinoma.
Mazziotti G, Sorvillo F, Piscopo M, Cioffi M, Pilla P, Biondi B, Iorio S, Giustina A, Amato G, Carella C. SourceDepartment of Clinical and Experimental Medicine, F. Magrassi & A. Lanzara, Second University of Naples, Naples, Italy.
Abstract
In women monitored for thyroid carcinoma, short-term stimulation with rhTSH induced an acute decrease in serum C-telopeptides of type-1 collagen and an increase in serum BALP levels without any effect on OPG production. The inhibitory effect of TSH on bone resorption occurred only in postmenopausal women who showed low BMD and a high bone turnover rate as an effect of L-thyroxine suppressive therapy.
INTRODUCTION: It has been recently shown that thyrotropin (TSH) has an inhibitory activity on skeletal remodeling in in vitro conditions. Here, we have aimed at evaluating whether TSH has similar effects in vivo. For this purpose, we have evaluated the sequential profile of serum bone metabolism markers during acute stimulation with recombinant human TSH (rhTSH) in thyroidectomized women monitored for thyroid carcinoma.
MATERIALS AND METHODS: The study group included 66 thyroidectomized patients, of whom 38 were premenopausal and 28 postmenopausal, who underwent routine rhTSH-assisted whole body radioactive iodine scanning for differentiated thyroid carcinoma. The patients were sequentially evaluated for TSH, free triiodothyronine (FT3), free thyroxine (FT4), bone alkaline phosphatase (BALP), C-telopeptides of type-1 collagen (CrossLaps), and osteoprotegerin (OPG) levels during rhTSH stimulation. The samples were drawn just before and 2 and 7 days after the first administration of rhTSH. BMD was evaluated by ultrasonography at baseline. Seventy-one healthy women (41 premenopausal and 30 postmenopausal) acted as a control group.
RESULTS AND CONCLUSIONS: At study entry, all patients had subclinical thyrotoxicosis as effect of L-thyroxine (L-T4) treatment. The patients had higher serum CrossLaps and OPG levels and lower BMD than healthy subjects. Postmenopausal patients showed comparable serum FT4 and FT3 concentrations with those found in premenopausal patients. However, postmenopausal patients showed higher serum CrossLaps (p < 0.001), OPG (p = 0.03), and BALP (p < 0.001) levels and lower BMD (p < 0.001) than those measured in premenopausal patients.
Two days after the first administration of rhTSH, all patients had serum TSH values >100 mUI/liter. At this time, serum CrossLaps levels decreased significantly (p < 0.001) and BALP values increased (p = 0.001) with respect to the baseline values in postmenopausal but not in premenopausal patients. rhTSH did not induce any significant change in serum OPG values either in premenopausal or in postmenopausal patients.
One week after the first rhTSH administration, serum CrossLaps values decreased again to values comparable with those measured at baseline, whereas serum BALP values remained high.
This study shows that subclinical thyrotoxicosis is accompanied by high bone turnover rate with an increase in serum OPG levels compared with euthyroid healthy subjects.
Acute increase in serum TSH levels is accompanied by a reversible inhibition of bone resorption. This effect is characterized by a decrease in serum CrossLaps and an increase in BALP levels without any evident effect on OPG production. The activity of TSH occurs specifically in postmenopausal women in whom the negative effects of L-T4 suppressive therapy on bone mass and metabolism are more marked compared with premenopausal women.
(19) http://www.ncbi.nlm.nih.gov/pubmed/19548061
J Bone Miner Metab. 2010;28(1):35-41. Epub 2009 Jun 23. The effects of recombinant human TSH on bone turnover in patients after thyroidectomy. Karga H, Papaioannou G, Polymeris A, Papamichael K, Karpouza A, Samouilidou E, Papaioannou P. Source2nd Division of Endocrinology and Metabolism, Alexandra Hospital, Vas. Sofias and Lourou, 11528 Athens, Greece.
Thyrotropin receptors are expressed in several extrathyroidal tissues including bone. We investigated whether the increase of thyroid-stimulating hormone (TSH) levels, under stable thyroid hormone levels, affects the bone markers.
Thirty-two postmenopausal women, with papillary thyroid carcinoma, previously treated with near-total thyroidectomy and I131 remnant ablation underwent routine evaluation for residual disease by using injections of recombinant human TSH (rhTSH) without withdrawal from thyroxine therapy. Changes in TSH levels and various serum and urine markers of bone metabolism were followed before and 1, 2, 5, and 7 days after the rhTSH injections.
A transient, significant decrease in serum calcium and urinary excretion of C- and N-terminal telopeptides of type I collagen was observed after the injections of rhTSH. Serum parathyroid hormone (PTH) started to rise along with TSH, but a significant increase of PTH was only reached on Day 5 when the TSH concentration had fallen more than 80% of the peak value. Bone alkaline phosphatase and osteocalcin did not show any significant change over time. There was no significant correlation between TSH concentration and the various parameters we measured. The study provides evidence that rhTSH produces a transient inhibition of bone resorption, as well as an attenuation of osteoblast response in spite of the PTH activation. Additional studies are needed to resolve the mechanisms by which TSH alters the response of the bone cells.
(20) Benefit of Estrogen-abolishes reduction in BMD from T4-Synthroid therapy
“Beneficial influence of estrogen replacement upon both BMD and fracture risk in postmenopausal women with a history of thyroid disease suggests that estrogen administration should be encouraged in this group.”
http://www.ncbi.nlm.nih.gov/pubmed/8563472
Thyroid. 1995 Oct;5(5):359-63.
Effect of estrogen replacement therapy upon bone mineral density in thyroxine-treated postmenopausal women with a past history of thyrotoxicosis. Franklyn JA, Betteridge J, Holder R, Sheppard MC. SourceDepartment of Medicine, University of Birmingham, Queen Elizabeth Hospital, Edgbaston, UK.
Abstract
We have shown that previous thyrotoxicosis and subsequent levothyroxine (L-T4) therapy are together associated with reduction in femoral and lumbar vertebral bone mineral density (BMD) in postmenopausal women. To determine whether estrogen replacement therapy exerts a beneficial effect upon bone loss in this situation, we performed a cross-sectional study comparing BMD measurements of the femur and lumbar spine in four groups of women (n = 15 in each group) matched for age and duration of menopause:
(i) those with a previous history of thyrotoxicosis who were subsequently receiving both L-T4 and estrogen replacement therapy for at least 3 years (L-T4 + HRT group),
(ii) previously thyrotoxic women matched to group (i) for L- dose and duration who had never used estrogen replacement (L-T4 alone group),
(iii) those with no history of thyroid disease who had received estrogen replacement therapy for at least 3 years (HRT alone group), and
(iv) those with no history of thyroid disease who had never received estrogen replacement therapy (control group).
BMD measurements were higher at each site in the HRT alone group than in controls (6.0-13.6% increases in BMD, p < 0.05 for measurements at femoral neck, Ward’s triangle, and trochanter) while measurements of BMD were lower at each site in the L-T4 alone group than in controls (3.3-6.1% reductions in BMD), although values did not reach statistical significance.
Measurements at each site in the L-T4 + HRT group were higher than those from the L-T4 alone group (2.2-16.1% increases in BMD, p < 0.05 for measurements at lumbar spine), although lower than in the group receiving HRT alone (p < 0.05 for femoral neck and Ward’s triangle) and similar to those in untreated controls.
Our results indicate that estrogen replacement therapy abolishes reduction in femoral and vertebral BMD in postmenopausal women with previous thyrotoxicosis and subsequent L-T4 therapy. This potentially beneficial influence of estrogen replacement upon both BMD and fracture risk in postmenopausal women with a history of thyroid disease suggests that estrogen administration should be encouraged in this group.
Low TSH and accelerated Bone Loss
http://www.ncbi.nlm.nih.gov/pubmed/2375563
Accelerated Bone Loss in Hypothyroid Patients Overtreated with L-Thyroxine
Annals of Internal Medicine August 15, 1990 vol. 113 no. 4 265-269
Glenn M. Stall, MD; Susan Harris, MS; Lori J. Sokoll, MCC; and Bess Dawson-Hughes, MD
Objective: To compare the rate of bone mineral loss in thyroxine-treated women with low thyrotropin (thyroid stimulating hormone, TSH) levels with that in women without known thyroid disease.
Design: Cases selected from a prospective calcium trial.
Setting: Subjects were recruited from the Boston area.
Measurements and Main Results: Of 361 women enrolled in a 2-year calcium supplement trial, 18 received thyroxine for hypothyroidism. Of these, 10 were considered overtreated, because they had low TSH levels. Rates of loss of bone mineral density from the radius, spine, and hip during 1.9 ± 0.6 years were measured by single- and dual-photon absorptiometry. When compared with women with no known thyroid disease (236 controls for the spine, 246 for the radius, and 237 for the femoral neck), women with low TSH levels had greater annualized, adjusted mean rates of bone loss from the spine (-2.89% ± 0.65% compared with -1.13% ± 0.13%, P = 0.009) and similar but not significant trends at the radius (-1.18% ± 0.75% compared with -0.13% ± 0.17%) and femoral neck (-1.39% ± 0.80% compared with -0.28% ± 0.19%). These means were adjusted for variables that affected the rate of loss in the control group (baseline bone mineral density and body mass index, calcium intake, and years since menopause). There were no statistical differences between the low TSH and control groups for any laboratory variables measured, including serum calcium, phosphorus, parathyroid hormone or alkaline phosphatase, plasma 25-hydroxyvitamin D or 1,25-dihydroxyvitamin D, or 24-hour urine calcium-to-creatinine ratio.
Conclusions: Thyroxine-treated women with low TSH levels lose bone mineral from the spine more rapidly than do women without known thyroid disease. These patients are therefore at increased risk for osteoporosis. The absence of detectable biochemical changes in women with low TSH levels may result from their relatively modest degree of overtreatment.
Hypothyroidism (High TSH) associated with adaptive reduced bone turn over which is restored to normal with a lower (euthyroid) TSH.
http://www.ncbi.nlm.nih.gov/pubmed/14727010
Osteoporos Int. 2004 Mar;15(3):209-16. Epub 2004 Jan 16.
Restoration of euthyroidism accelerates bone turnover in patients with subclinical hypothyroidism: a randomized controlled trial.
Meier C, Beat M, Guglielmetti M, Christ-Crain M, Staub JJ, Kraenzlin M.
SourceDivision of Endocrinology, Department of Medicine, University Hospitals, CH-4031, Basel, Switzerland. cmeier@med.usyd.edu.au
Abstract
This study evaluated the effect of physiological l-thyroxine (L-T4) treatment on bone metabolism in patients with subclinical hypothyroidism. Sixty-six women with subclinical hypothyroidism (TSH 11.7 +/- 0.8 mIU/l) were randomly assigned to receive L-T4 or placebo for 48 weeks. Sixty-one of 66 patients completed the study. Individual L-T4 replacement (mean dosage 85.5 +/- 4.3 microg/day) was performed targeting euthyroid thyroid-stimulating hormone (TSH) levels. The primary outcome measure was 24- and 48-week change in markers of bone formation (total and bone alkaline phosphatase [ALP, bone ALP], osteocalcin [OC]) and resorption (pyridinoline [PYD] and deoxypyridinoline [DPD], C-terminal cross-linking telopeptide type I [CTX]). Secondary outcomes were 48-week changes in bone mineral density (BMD) of the lumbar spine and hip, measured by dual-energy X-ray absorptiometry. Compared with placebo, l-thyroxine ( n=31) resulted in significant activation of bone turnover. Overall, a significant treatment effect was observed for DPD (between-group difference 16.0%; 95%CI, 10.9 to 21.1), CTX (29.9%; 95%CI, 23.3 to 36.5), and bone ALP (13.2%; 95%CI, 6.6 to 19.7) after 24 weeks. At the end of the study, lumbar BMD in the both treatment groups differed by 1.3% (95%CI, -2.9 to 0.5) with lower levels in l-thyroxine treated women. Significant difference in BMD between groups was also observed at the trochanter. We conclude that physiological l-thyroxine treatment accelerates bone turnover reflecting early activation of bone remodeling units in the initial replacement of subclinical hypothyroidism. The observed bone loss could be interpreted as an adaptive mechanism on decreased bone turnover in preexistent hypothyroidism, and not as l-thyroxine-induced clinically important bone loss. However, long-term studies are needed to confirm this assumption.
No Change in BMD when Synthroid dose adjusted down for pats with suppressed TSH.
http://www.ncbi.nlm.nih.gov/pubmed/9156039
Clin Endocrinol (Oxf). 1997 Mar;46(3):301-7.
Longitudinal changes of bone mineral density and bone turnover in postmenopausal women on thyroxine. Guo CY, Weetman AP, Eastell R. SourceDepartment of Human Metabolism and Clinical Biochemistry, University of Sheffield, Northern General Hospital, UK.
Abstract
OBJECTIVE: The skeletal risks of subclinical hyperthyroidism in postmenopausal women on replacement thyroxine remain controversial. The aims of this study were to determine (1) the relationship between bone turnover and TSH levels and (2) whether reduction of thyroxine (T4) dose in postmenopausal women who have suppressed TSH levels is beneficial to bone mineral density (BMD) and bone turnover.
DESIGN: A prospective study over 2 years of post-menopausal women treated with T4 with an age- and sex-matched healthy control group.
PATIENTS AND MEASUREMENTS: Sixty-four post-menopausal women, ages 47 to 74 (61 +/- 9, mean +/- SD), on T4 for between 2 and 14 years.
Patients were divided into three groups: group 1 (n = 23) with normal serum TSH levels, group 2 (n = 18) with suppressed serum TSH levels and group 3 (n = 23) with a history of thyroidectomy and suppressed TSH levels (patients with thyroid cancer). Thirty-six age-matched healthy postmenopausal women were recruited as a control group. Bone mineral density (BMD), measured by dual-energy X-ray absorptiometry and bone turnover, were evaluated at baseline and over 2 years in the four groups. Serum TSH levels were measured every 6 to 12 months. In group 2, the dose of T4 was reduced after the baseline measurement and serum TSH levels were remeasured 1 to 4 months later. Serum TSH levels returned to the reference range after the reduction of T4 dose in group 2.
RESULTS: The serum TSH level, after log transformation, was negatively correlated with serum levels of osteocalcin (BGP), bone alkaline phosphatase (BAP) and urinary cross-linked N-telopeptides pyridinoline of type I collagen (NTx) (linear correlation, r = -0.41 P < 0.001, r = -0.29 P = 0.01 and r = -0.26 P = 0.033), respectively.
There was no significant difference in BMD and bone turnover between the four groups at either baseline or follow-up (ANOVA, P > 0.05). The levels of serum BGP, BAP and urinary NTx decreased whereas lumbar spine and femoral neck BMD increased significantly in group 2 over 2 years (one sample t-test, P = 0.0021, 0.034, 0.0017, 0.011 and < 0.001, respectively). In group 2, the rates of change of lumbar spine and femoral BMD were increased significantly and the rates of change of serum BGP and urinary NTx were decreased significantly compared with other groups (Scheffe test, P < 0.05).
CONCLUSIONS: In postmenopausal women on T4, bone turnover is related to the serum TSH level and a reduction of T4 dose in those with suppressed serum TSH levels can result in a decrease in bone turnover and an increase in bone mineral density.
BMD correlates with TSH level
http://www.ncbi.nlm.nih.gov/pubmed/20429634
Endocr Regul. 2010 Apr;44(2):57-63.
Thyrotropin versus thyroid hormone in regulating bone density and turnover in premenopausal women. Baqi L, Payer J, Killinger Z, Hruzikova P, Cierny D, Susienkova K, Langer P. 5th Clinic of Internal Medicine, Faculty of Medicine, Comenius University, Bratislava, Slovakia.
Abstract
OBJECTIVE: This cross-sectional study aimed to evaluate the interrelations between endogenous TSH level on one side and the status of bone mineral density (BMD) and bone metabolic turnover (BMT) on the other in pooled four groups of premenopausal women either without or with a long-term L-thyroxine treatment.
METHODS: Serum levels of free thyroxine (FT4), thyrotropin (TSH), calcium (Ca), alkaline phosphatase (ALP), osteocalcin (OC) and cross linked N-telopeptide of type 1 collagen (NTx) as well as urinary calcium (U-Ca/24h), bone mineral density of lumbar spine L 1-4 (BMD-L) and femoral hip (BMD-F) were estimated in a cohort of 151 premenopausal women (median 36 years) consisting of four groups:
Group 1, 40 healthy untreated women, while three other groups consisted of patients previously treated for about 5 years;
Group 2, 41 patients with genuine hypothyroidism treated by L-thyroxine (50-100 microg daily);
Group 3, 40 patients with genuine hyperthyroidism treated by Carbimazol (10-15 mg daily);
Group 4, 30 patients treated by suppressive doses of L-thyroxine (100-150 microg daily) after thyroidectomy for thyroid cancer (n=10) or because of progressively growing benign goitre (n=20).
RESULTS: When using multiple correlation analysis (Pearson’s r) in pooled 151 women, TSH showed significant positive correlation with BMD-L (p<0.01) and BMD-F (p<0.001) and, at the same time, significant negative correlation with serum level of BMT markers such as ALP (p<0.05), OC (p<0.05) and NTx (p<0.01), while the correlation of FT4 with BMD-L, BMD-F was significantly negative (p<0.001 for both) and that with all BMT markers was significantly positive (p<0.05 to <0.001).
Thus, it appeared that higher TSH level was associated with increased bone mineral density and, at the same, with decreased bone metabolic turnover. These interrelations were further supported by the findings of significantly lower BMD-F (p<0.01), BMD-L (p<0.001) and significantly higher ALP, OC and NTX (all at p<0.001) in the group of 36 women with TSH level<0.3 mU/l as compared to the group of 115 women with TSH level range of 0.35-6.3 mU/l).
CONCLUSIONS: Irrespectively of thyroid diagnosis and/or previous long term thyroxine treatment in some groups, this cross sectional study showed that, after the pooled group of 151 women has been redistributed according to the actual TSH level, the bone mineral density and the level of bone turnover markers was significantly more favorable in 115 subjects with TSH level range of 0.35-6.3 mU/l than these in 36 women with TSH<0.3 mU/l.
Combination of Synthroid and Cytomel showed higher activation of bone resorption
http://www.ncbi.nlm.nih.gov/pubmed/20688622
Hormones (Athens). 2010 Jul-Sep;9(3):245-52. Combined therapy with L-thyroxine and L-triiodothyronine compared to L-thyroxine alone in the treatment of primary hypothyroidism. Fadeyev VV, Morgunova TB, Melnichenko GA, Dedov II. Department of Endocrinology, Moscow Medical Academy, Moscow, Russia.
OBJECTIVE: The objective of this study was to compare various parameters in patients with hypothyroidism receiving either monotherapy with L-thyroxine (L-T4) or combination therapy with L-T4 and L-triiodothyronine (L-T3).
DESIGN: We conducted a randomized, controlled trial in 36 premenopausal women with hypothyroidism. The patients were divided into two groups:
Group A (n=20) received only L-T4, while
Group B received the combination L-T4 and L-T3.
The treatment period lasted for 6 months.
RESULTS: At baseline, the various parameters examined did not differ in the two groups. No significant difference between monotherapy and combined therapy was demonstrated on TSH level, ECG monitoring, densitometry, or thyroid symptoms score. The lipid profile was better during combined treatment compared to L-T4 alone; in Group A during treatment with L-T4 the levels of cholesterol and low density lipoprotein (LDL) cholesterol were unchanged, while in group B total cholesterol and LDL decreased (p<0.05). The changes in osteocalcin levels did not differ in the two groups, whereas the levels of urine deoxypyridinoline at the end of therapy were higher in the group with combination therapy, compared to monotherapy.
CONCLUSION: Compared with L-T4 alone, replacement therapy with the combination of L-T4+L-T3 shows favourable changes in serum lipid profile, but higher activation of bone resorption.
Low TSH associated with higher bone turnover in GD. Anti-TSH receptor ABS a sensitive indicator of increased bone turnover
http://www.ncbi.nlm.nih.gov/pubmed/11095447
J Clin Endocrinol Metab. 2000 Nov;85(11):4157-61.
Persistent increase in bone turnover in Graves’ patients with subclinical hyperthyroidism.
Kumeda Y, Inaba M, Tahara H, Kurioka Y, Ishikawa T, Morii H, Nishizawa Y.
SourceDepartment of Internal Medicine, Osaka City University Graduate School of Medicine, Japan.
Abstract
Hyperthyroid patients exhibit accelerated bone loss by increased bone turnover, and normalization of thyroid function is associated with a significant attenuation of increased bone turnover, followed by an increase in bone mineral density. However, of patients with Graves’ disease (GD) maintained on antithyroid drug (ATD) treatment, some exhibit persistent suppression of TSH long after normalization of their serum free T3 (FT3) and free T4 (FT4) levels. The aim of this study was to examine whether bone metabolism is still enhanced in
TSH-suppressed premenopausal GD patients with normal FT3 and FT4 levels after ATD therapy (n = 19) compared with that in
TSH-normal premenopausal GD patients (n = 30),
and to evaluate the relationship between serum TSH receptor antibody (TRAb), an indicator of disease activity of GD, and various biochemical markers of bone metabolism.
No difference was found between the two groups in serum Ca, phosphorus, or intact PTH, or in urinary Ca excretion.
Serum bone alkaline phosphatase (B-ALP), bone formation markers, and urinary excretions of pyridinoline (U-PYD) and deoxypyridinoline (U-DPD), which are bone resorption markers, were significantly higher in the TSH-suppression group than in the TSH-normal group (B-ALP, P < 0.05; U-PYD, P < 0.001; U-DPD, P < 0.001).
For the group of all GD patients enrolled in this study, TSH, but neither FT3 nor FT4, exhibited a significant negative correlation with B-ALP (r = -0.300; P < 0.05), U-PYD (r = -0.389; P < 0.05), and U-DPD (r = -0.446; P < 0.05), whereas TRAb exhibited a highly positive and significant correlation with B-ALP (r = 0.566; P < 0.0001), U-PYD (r = 0.491; P < 0.001), and U-DPD (r = 0.549; P < 0.0001). Even in GD patients with normal TSH, serum TRAb was positively correlated with B-ALP (r = 0.638; P < 0.001), U-PYD (r = 0.638; P < 0.001), and U-DPD (r = 0.641; P < 0.001).
In conclusion, it is important to achieve normal TSH levels during ATD therapy to normalize bone turnover. TRAb was not only a useful marker for GD activity, but was also a very sensitive marker for bone metabolism in GD patients during ATD treatment.
Only patients with full TSH suppression in the postmenopausal group showed a tendency to lower BMD.
http://www.ncbi.nlm.nih.gov/pubmed/15278189
J Formos Med Assoc. 2004 Jun;103(6):442-7.
Bone mineral density in women receiving thyroxine suppressive therapy for differentiated thyroid carcinoma. Chen CH, Chen JF, Yang BY, Liu RT, Tung SC, Chien WY, Lu YC, Kuo MC, Hsieh CJ, Wang PW. Department of Internal Medicine, Chang Gung Memorial Hospital, Kaohsiung, Taiwan.
Abstract
BACKGROUND AND PURPOSE: Most patients with well-differentiated thyroid carcinoma have an excellent prognosis and are likely to live long enough to be subjected to osteoporosis. The purpose of this study was to investigate the consequences of treatment with a supraphysiological dose of levothyroxine (l-T4) on bone mineral density (BMD) in Taiwanese women with differentiated thyroid cancer.
METHODS: A total of 69 (44 premenopausal, 25 postmenopausal) Taiwanese women with differentiated thyroid cancer were included in this retrospective study. These patients were free of disease recurrence after initial near-total thyroidectomy and I-131 radioablation, and had undergone regular l-T4 suppressive therapy for more than 3 years (mean, 7.3 +/- 3.0 years; range, 3 to 15 years). The degree of thyroid-stimulating hormone (TSH) suppression was determined based on the mean TSH score for each patient which was determined by analysis of all available follow-up TSH data, where
1 = undetectable TSH (< 0.2 mIU/mL);
2 = subnormal TSH (0.2 to 0.39 mIU/mL);
3 = normal TSH (0.4 to 4.0 mIU/mL); and
4 = elevated TSH (> 4.0 mIU/mL).
The patients were divided into a full TSH suppression group with a mean TSH score in the range 1.0 to 1.99, and a partial TSH suppression group with a mean TSH score in the range 2.0 to 2.99. BMD was measured by dual-energy X-ray absorptiometry at the lumbar spine, femoral neck, Ward’s triangle and total hip. Comparisons between subgroups of patients and controls were performed by unpaired t test. Correlation between BMD and other clinical variables was assessed by Pearson’s correlation analysis.
RESULTS: Postmenopausal patients (aged 57.7 +/- 6.9 years) had significantly higher serum calcium levels and decreased BMD at all sites of the spine and hip as compared with premenopausal patients (aged 38.6 +/- 6.7 years) with similar BMI and duration of TSH suppression. Comparison of BMD between postmenopausal patients and BMI- and age-matched controls revealed that the patient group had decreased BMD at all sites of measurement, although this difference was not significant. This phenomenon was not observed in the premenopausal patients. Furthermore, when BMD was compared between patients categorized as having full and partial suppression of TSH, only patients with full suppression in the postmenopausal group showed a tendency to lower BMD. There was a strong correlation of BMD with age, BMI and serum calcium level. However, no correlation was found between BMD and degree of TSH suppression or duration of l-T4 suppression therapy.
CONCLUSION: Women with differentiated thyroid cancer who had long-term (mean, 7.3 +/- 3.0 years) l-T4 therapy and suppressed TSH levels had no evidence of lower BMD. However, patients with full suppression in the postmenopausal group showed a tendency towards lower BMD. Therefore, careful monitoring of BMD in postmenopausal women during suppression therapy is mandatory.
BMD lower in post thyroidectomy patients on T4
http://www.ncbi.nlm.nih.gov/pubmed/16834835
Curr Med Res Opin. 2006 Jul;22(7):1369-73.
Changes of bone mineral density in pre-menopausal women with differentiated thyroid cancer receiving L-thyroxine suppressive therapy.
Mazokopakis EE, Starakis IK, Papadomanolaki MG, Batistakis AG, Papadakis JA.
SourceDepartment of Internal Medicine, University Hospital of Heraklion, Crete, Greece.
OBJECTIVE: We studied the effect of levothyroxine (L-T(4)) suppressive therapy on bone mineral density (BMD) in pre-menopausal women with total thyroidectomy and radioactive iodine ((131)I) ablation therapy post-operatively for differentiated thyroid cancer (DTC).
PATIENTS AND METHODS: We prospectively studied 26 athyroid pre-menopausal women (median age 39 years, range 28-48 years) receiving suppressive L-T(4) therapy postoperatively for 48 months. BMD was measured by dual energy X-ray absorptiometry (DEXA) at the femoral neck, femoral trochanter and Ward’s triangle, before (basal) and during (12th and 48th month) the follow-up period. None of the women gave a medical history that could possibly affect bone metabolism. Patients were free of thyroid cancer in clinical and laboratory examinations at the time of the study. Paired t-test was used for comparisons among BMD measurements during the suppressive therapy.
RESULTS: There were statistically significant decreases of BMD at all measured regions during (12th and 48th month) L-T(4) suppressive therapy. The overall decreases in BMD at the femoral neck, femoral trochanter and Ward’s triangle were 7.5%, 10.9% and 3.4%, respectively, at the end of the follow-up period. The coefficient of variation (CV) of all BMD measurements was around 10%, showing a rather homogenous group of patients. Our patients had a statistically significant decrease in their body mass index (BMI) and weight at the end of the follow-up period. However, there was no significant correlation between the decrease in BMI and BMD. Patients did not experience significant adverse effects from L-T(4) suppressive therapy during the study.
CONCLUSION: L-T(4) suppressive therapy for at least 1 year in pre-menopausal women with DTC causes a reduction in BMD of the femoral neck, femoral trochanter and Ward’s triangle.
Lower TSH associated with increased risk of hip fracture
http://www.ncbi.nlm.nih.gov/pubmed/12803168
Ann Intern Med. 2001 Apr 3;134(7):561-8.
Risk for fracture in women with low serum levels of thyroid-stimulating hormone.
Bauer DC, Ettinger B, Nevitt MC, Stone KL; Study of Osteoporotic Fractures Research Group. University of California, San Francisco, 74 New Montgomery, Suite 600, San Francisco, CA 94105, USA.
Abstract
BACKGROUND: Biochemical evidence of hyperthyroidism may be associated with low bone mass, particularly in older postmenopausal women, but no prospective studies of thyroid function and subsequent fracture risk have been done.
CONCLUSIONS: Women older than 65 years of age who have low serum TSH levels, indicating physiologic hyperthyroidism, are at increased risk for new hip and vertebral fractures. Use of thyroid hormone itself does not increase risk for fracture if TSH levels are normal.
———————————————————————–
Are these studies missing the Hashimotos cases with C cell destruction, low calcitonin and high thyroid function with low TSH?
LOW TSH correllated with increased fracture risk in post menopausal women with low bone density
http://www.ncbi.nlm.nih.gov/pubmed/19892039?dopt=Abstract
Bone. 2010 Mar;46(3):747-51. Epub 2009 Nov 3.
Serum TSH values and risk of vertebral fractures in euthyroid post-menopausal women with low bone mineral density. Mazziotti G, Porcelli T, Patelli I, Vescovi PP, Giustina A.
SourceDepartment of Medical and Surgical Sciences, University of Brescia, Italy.
Abstract
INTRODUCTION: There is evidence that variations of thyrotropin (TSH) even in its reference range may influence bone mineral density (BMD). In fact, low-normal TSH values have been associated with high prevalence of osteoporosis in post-menopausal women. However, data associating TSH and risk of fractures are scanty and limited to subjects with subclinical thyrotoxicosis.
MATERIALS AND METHODS: In this observational study, we investigated the correlation between serum TSH and prevalence of radiological vertebral fractures in a cohort of 130 post-menopausal women with normal thyroid function.
RESULTS: Osteoporosis was observed in 80 women (61.5%), whereas 49 women (37.7%) had osteopenia. Vertebral fractures were found in 49 women (37.7%), who were significantly older, with higher prevalence of osteoporosis and with lower serum TSH values as compared with women who did not fracture. Stratifying the patients according to serum TSH values, vertebral fractures were found to be significantly (p=0.004) more prevalent in first tertile (56.8%) of TSH values as compared with the second (23.3%) and third tertiles (32.6%). Multivariate logistic regression analysis demonstrated that low serum TSH maintained a significant correlation with vertebral fractures (odds ratio 2.8, C.I. 95% 1.20-6.79) even after correction for age, BMD, BMI and serum free-thyroxine values.
DISCUSSION: Low-normal TSH values are associated with high prevalence of vertebral fractures in women with post-menopausal osteoporosis or osteopenia, independently of thyroid hormones, age and BMD.
—————————————————————–
Hyperthyrodism yes, but not Thyroxine associated with Hip Fracture
http://www.ncbi.nlm.nih.gov/pubmed/7891045?dopt=Abstract
J Intern Med. 1995 Mar;237(3):241-7.
Hip fractures and the thyroid: a case-control study. Wejda B, Hintze G, Katschinski B, Olbricht T, Benker G. SourceDepartment of Clinical Endocrinology, Medizinische Klinik und Poliklinik, University of Essen, Germany.
Abstract
OBJECTIVE: To investigate the prevalence of thyroid illness – especially hyperthyroidism – and exposure to thyroid hormones in patients with hip fracture. DESIGN: A case-control study. SETTING: Two surgical/orthopaedic hospital units and 22 facilities for the aged in a moderately iodine-deficient region of Germany.
SUBJECTS: A total of 116 postmenopausal females with hip fracture and 402 postmenopausal female controls.
MAIN OUTCOME MEASURES: Hip fracture; thyroid disease confirmed by measurement of serum thyrotropin, total and free thyroxine and triiodothyronine; history of thyroid disease and thyroid medication obtained by a questionnaire.
RESULTS: Of the hip fracture patients 4.3% had overt untreated hyperthyroidism, and 6.9% gave a history of past hyperthyroidism (total, 11.2%). The corresponding figures for the controls were 2.0 and 2.7%, respectively (total, 4.7%). 7.8% of the cases had been exposed to levo-thyroxine for 3-29 years, compared to 11.2% of the controls. The odds ratio for hyperthyroidism (present and past) was 2.5 (1.2-5.3, 95% confidence interval), and the odds ratio for levo-thyroxine exposure was 0.67 (0.32-1.41) in the hip fracture patients.
CONCLUSIONS: Hyperthyroidism is found 2.5-fold more often in hip fracture patients than in controls. Hence, hyperthyroidism appears to be a significant risk factor for hip fracture and should be investigated by clinical and, when necessary, laboratory means in hip fracture patients. In contrast, no increased risk for hip fracture could be detected after exposure to levothyroxine.
NO effect of thyroxine on Bone Density
http://www.ncbi.nlm.nih.gov/pubmed/9579237
Clin Endocrinol (Oxf). 1998 Feb;48(2):229-34.
Effect of replacement doses of thyroxine on bone mineral density. Hanna FW, Pettit RJ, Ammari F, Evans WD, Sandeman D, Lazarus JH. Department of Medicine, University of Wales College of Medicine, Cardiff, UK.
Abstract
INTRODUCTION: Hyperthyroidism is associated with a reduction in bone mineral density (BMD). Suppressive doses of thyroxine (T4), inducing subclinical hyperthyroidism, have been reported by some investigators to reduce BMD. Little work has been done on replacement doses of T4. AIM: The aim was to investigate the effect of replacement doses of T4 on BMD. STUDY DESIGN: Cross-sectional study of hypothyroid patients on long-term T4 replacement doses, comparing those who had primary hypothyroidism with those who were previously hyperthyroid.
PATIENTS: Fifty women on replacement doses of T4 for more than 5 years were recruited. Twenty-five were treated for primary (group 1) and 25 for radioiodine-induced hypothyroidism (group 2). They were well matched for age, menstrual status, smoking history, body mass index (BMI), dose and duration of T4 replacement as well as thyroid status.
MEASUREMENTS: BMD was assessed by dual energy X-ray absorptiometry. Free T4 (FT4), FT3 as well as ultrasensitive TSH assays were used to assess thyroid status.
RESULTS: The two groups showed no difference in BMD (g/cm2) of the lumbar spine (1.008 vs. 0.957, P = 0.25), femoral neck (0.745 vs. 0.735, P = 0.79) and total hip (0.878 vs. 0.837, P = 0.24). When the two groups were pooled, there was no significant difference between the patients and a reference population with femoral neck and total hip BMD expressed as a standard deviation (Z) score. However, the lumbar spine mean Z score was significantly greater than zero. For each site, there was a negative correlation of BMD with age in at least one group but, in general, BMI, FT4, FT3 and duration of T4 replacement did not correlate with BMD. T4 dose, however, had a consistent positive correlation with BMD in the spine, femoral neck and the hip (P = 0.01, 0.04 and 0.02, respectively) in group 2 but not group 1.
CONCLUSION: In this study, there is no evidence for a difference in bone mineral density in patients receiving replacement doses of thyroxine irrespective of the aetiology of their hypothyroidism. The reduced bone mineral density associated with hyperthyroidism appears to be restored, maintained and in some cases possibly improved while on long-term thyroxine replacement post-radioiodine.
http://www.ncbi.nlm.nih.gov/pubmed/15555712
J Affect Disord. 2004 Dec;83(2-3):183-90.
Bone mineral density during maintenance treatment with supraphysiological doses of levothyroxine in affective disorders: a longitudinal study.
Bauer M, Fairbanks L, Berghöfer A, Hierholzer J, Bschor T, Baethge C, Rasgon N, Sasse J, Whybrow PC. SourceDepartment of Psychiatry and Psychotherapy, Charité-University Medicine Berlin, Campus Charité Mitte, Berlin, Germany.
BACKGROUND: This prospective study was designed to determine whether patients with prophylaxis-resistant affective disorders, receiving adjunctive maintenance therapy with supraphysiological doses of levothyroxine (L-T4), show evidence of accelerated bone loss compared to the reference population database.
METHODS: In 21 patients, bone mineral density (BMD) of the spine (lumbar vertebrae L1-L4) and femur (femoral neck, trochanter, and Ward’s triangle) was measured by dual energy X-ray absorptiometry (DXA). BMD measurement was performed first after patients had been on thyroid-stimulating hormone (TSH)-suppressive therapy with L-T4 (mean dose=411 mcg/d) for an average of 16.4 months and again after 33.6 months of L-T4 (mean dose=416 mcg/d) therapy.
RESULTS: There was no statistically significant difference between the actual percentage decline in bone mineral density and the expected percentage decline in any of the measured bone regions. In a stepwise linear regression analysis, age was identified as a predictor of percentage change in BMD. After controlling for age, the only other variable that showed a consistent trend was the dose of L-T4, with higher doses being positively correlated with the percentage decline of BMD.
LIMITATIONS: Relatively small sample size, no bone density assessment prior to treatment with L-T4, no patient control group with mood disorders who did not receive L-T4 treatment, and bone density follow-up intervals were variable.
CONCLUSIONS: This study did not demonstrate evidence that long-term treatment of affectively ill patients with supraphysiological doses of L-T4 significantly accelerates loss of bone mineral density compared to the age-matched reference population. However, the decline of BMD in one individual patient underscores that caution is indicated and that regular assessment of BMD during longer-term supraphysiological thyroid hormone treatment is needed.
http://www.ncbi.nlm.nih.gov/pubmed/11578671
J Affect Disord. 2001 Oct;66(2-3):185-91.
Bone mineral density in pre-and post-menopausal women with affective disorder treated with long-term L-thyroxine augmentation. Gyulai L, Bauer M, Garcia-Espana F, Hierholzer J, Baumgartner A, Berghöfer A, Whybrow PC. Department of Psychiatry, Bipolar Disorders Unit, University of Pennsylvania Medical Center, 3600 Market Street, Room 800, Philadelphia, PA 19104, USA.
BACKGROUND: Augmentation with TSH-suppressive L-thyroxine (T4) has been shown to improve the course of illness in otherwise refractory affective disorders. This collaborative study investigates whether T4 augmentation for a minimum of 12 months decreases bone mineral density (BMD) in 26 pre- and post-menopausal women with affective disorder.
METHODS: We measured BMD at the femoral neck, Ward’s triangle, trochanter and lumbar vertebrae (L1-L4) in 13 premenopausal and 13 postmenopausal women with affective disorder using dual energy X-ray absorptiometry. BMD was expressed as g/cm(2) and as a Z-score, calculated using bone density data from the international reference population standard.
RESULTS: The Z-scores for the pre- and post-menopausal women were within the reference range of the age and sex matched population standard. BMD for the composite group also did not differ either from the population standard. BMD in the lumbar spine and hip did not differ significantly between the pre- and post-menopausal groups. However, there were a relatively high number of postmenopausal patients with BMDs one S.D. lower than the population standard.
LIMITATIONS: This is a cross-sectional study with a relatively small sample size.
CONCLUSIONS: The study demonstrates that T4 augmentation treatment does not reduce BMD to a clinically significant degree in many women with affective disorder. However, the resilience of bone structure to T4 treatment may vary with site and menopausal status. This study underscores the need for regular assessment of BMD during adjunctive thyroid treatments for affective disorder, especially in postmenopausal women.
http://www.ncbi.nlm.nih.gov/pubmed/14748891
J Clin Pharm Ther. 2004 Feb;29(1):1-5. Effects of levothyroxine suppressive therapy on bone mineral density in premenopausal women. Larijani B, Gharibdoost F, Pajouhi M, Sadjadi A, Aghakhani S, Eshraghian R, Akrami SM, Maalouf G. SourceInternal Medicine, Tehran University of Medical Sciences, Tehran, Iran.
BACKGROUND: Levothyroxine (L-T4) is widely prescribed for treating thyroid disorders, but its effect on bone mineral density (BMD), is being debated.
OBJECTIVES: We studied the effect of supraphysiologic doses of L-T4 on BMD in a group of premenopausal women.
PATIENTS AND METHODS: We included 50 women (mean age=36.8 +/- 7.6 years) receiving L-T4 for at least 1 year for treating their benign cold thyroid nodules. Serum T3, T4, thyroid-stimulating hormone (TSH), parathyroid hormone (PTH), calcium, and phosphate and urine calcium and sodium levels of all patients were measured. Bone density at femoral neck and lumbar (L1-L4) regions was measured, using dual energy X-ray absorptiometry (DXA).
RESULTS: No significant decrease was detected in the bone density of the subjects treated with L-T4 compared with the control group.
CONCLUSION: L-T4 treatment for 1 year is not associated with increased risk of osteoporosis in premenopausal women but other potential adverse effects still need to be monitored in women receiving L-T4 especially long-term.
http://www.ncbi.nlm.nih.gov/pubmed/7647577
Thyroid. 1995 Apr;5(2):81-7. Possible limited bone loss with suppressive thyroxine therapy is unlikely to have clinical relevance. Müller CG, Bayley TA, Harrison JE, Tsang R.
SourceDepartment of Medicine University of Toronto, St. Joseph’s Health Centre, Princess Margaret Hospital, Canada.
Abstract
To determine the effect of suppressive doses of thyroxine (T4) on bone mass, we studied 50 women on suppressive doses of T4 for 3-27 years (mean of 11 years).
Twenty-five had nontoxic goiter and
25 had well-differentiated thyroid carcinoma.
Fifty controls were matched for age, menopausal status, and body mass index.
Bone mineral density (BMD) was measured in the lumbar spine (LS), femoral neck (FN), trunk (TK), and extremities (EXT) by dual-energy X-ray absorptiometry (DXA). In addition, the trunk area was measured by neutron activation analysis and recorded as a calcium bone index (CaBI). Twenty-one patients were restudied with DXA measurements at a mean of 1.5 +/- 0.5 (1 SD) years.
The total population of 50 patients showed no difference in bone mass from controls. In patients with nontoxic goiter, there was no evidence of any loss in bone mass.
Cancer patients showed insignificant reductions of 2-5% in BMD of LS, FN, and TK and a significant 5% reduction in BMD of EXT, compared to controls, and a 12% reduction in CaBI compared to goiter patients. Cancer patients had a slightly higher (p < 0.001) mean daily dose of T4 than goiter patients (0.23 vs 0.15 mg/day) but had a similar degree of TSH suppression. BMD and CaBI values did not correlate with free T4 index) with the daily T4 dose, accumulative dose, or with duration of T4 therapy. There were no significant changes in bone mass in either goiter or cancer patients restudied after a mean of 1.5 years.
http://www.ncbi.nlm.nih.gov/pubmed/16322336
Endocr Relat Cancer. 2005 Dec;12(4):973-81.
Lack of deleterious effect on bone mineral density of long-term thyroxine suppressive therapy for differentiated thyroid carcinoma. Reverter JL, Holgado S, Alonso N, Salinas I, Granada ML, Sanmartí A. SourceDepartment of Endocrinology and Nutrition, Germans Trias i Pujol Hospital, Barcelona, Spain.
The effect of subclinical hyperthyroidism on bone mineral density is controversial and could be significant in patients with differentiated thyroid carcinoma who receive suppressive doses of levothyroxine (LT4). To ascertain whether prolonged treatment with LT4 to suppress thyrotropin had a deleterious effect on bone mineral density and/or calcium metabolism in patients thyroidectomized for differentiated thyroid cancer we have performed a cross-sectional study in a group of 88 women (mean +/- SD age: 51 +/- 12 years) treated with LT4 after near-total thyroidectomy and in a control group of 88 healthy women (51 +/- 11 years) matched for body mass index and menopausal status. We determined calcium metabolism parameters, bone turnover marker N-telopeptide and bone mass density by dual-energy X-ray absorptiometry. No differences were found between patients and controls in calcium metabolism parameters or N-telopeptide except for PTH, which was significantly increased in controls.
No differences were found between groups in bone mineral density in femoral neck (0.971 +/- 0.148 gr/cm(2) vs 0.956 +/- 0.130 gr/cm(2) in patients and controls respectively, P = 0.5). In lumbar spine, bone mineral density values were lower in controls than in patients (1.058 +/- 0.329 gr/cm(2) vs 1.155 +/- 0.224 gr/cm(2) respectively, P < 0.05). When premenopausal (n = 44) and postmenopausal (n = 44) patients were compared with their respective controls, bone mineral density was similar both in femoral neck and lumbar spine. The proportion of women with normal bone mass density, osteopenia and osteoporosis in patient and control groups was similar in pre- and postmenopausal women.
In conclusion, long-term suppressive LT4 treatment does not appear to affect skeletal integrity in women with differentiated thyroid carcinoma.
————-
Osteoporosis after thyroidectomy and T4 therapy
http://www.ncbi.nlm.nih.gov/pubmed/11698925
Medscape Womens Health. 2001 Oct;6(5):3. Bone loss in premenopausal women on long-term suppressive therapy with thyroid hormone. Sijanovic S, Karner I. SourceDepartment of Gynecology and Obstetrics, University Hospital Osijek, Osijek, Croatia.
Abstract
BACKGROUND: The effects on bone metabolism of long-term treatment with thyroid hormone given at suppressive doses have been debated.
OBJECTIVE: To determine whether long-term thyroxine therapy in the premenopausal period is a risk factor for the development of secondary osteoporosis and whether women receiving this therapy have increased bone loss during the premenopausal period.
PATIENTS AND METHODS: The study enrolled a select group of 19 premenopausal women of mean ages 39 +/- 8 years suffering from differentiated thyroid gland carcinoma. All subjects had undergone total thyroidectomy and subsequently initiated thyroxine suppressive therapy. At the beginning of our study, the women had been on suppressive therapy for 9.4 +/- 6.4 years. Laboratory results were performed to exclud other possible factors for secondary osteoporosis. This prospective study of bone mineral density (BMD) was conducted over a 4-year period on all subjects using the method of dual photon x-ray absorptiometry (DXA) of the spine and the femoral neck and also by the method of single-photon absorptiometry (SPA) of the distal radius.
RESULTS: At the beginning of this study, 2 subjects had osteopenia in the spine and 2 had osteopenia in the femoral neck; they had been on suppressive thyroxine therapy for 10 years. Osteopenia in the distal radius was found in 4 subjects. Overall, 8 of the 19 women had osteopenia at the beginning of the study. One year later, after the second BMD measurement, no statistically significant loss of bone mass occurred in any region of the skeleton in any of the patients. However, a review of the individual scores revealed osteopenia in 6 patients at the distal radius; bone loss also occurred at the spine and the femoral neck in several women, but not to the extent that would establish osteopenia. After the 4 years, BMD measurements indicated significant bone loss.
CONCLUSION: Our results suggest that women who begin long-term ( ~ 10 years) thyroxine therapy in the premenopausal period can develop osteopenia by the beginning of menopause.
————————————
it is the TSH hormone that inhibits bone resorption by direct effect on bone
http://joe.endocrinology-journals.org/cgi/reprint/204/1/13.pdf
REVIEW – TSH receptor activation and body composition . Anna de Lloyd1,*, James Bursell2,*, John W Gregory2, D Aled Rees1 and Marian Ludgate1 1Centre for Endocrine and Diabetes Sciences and 2Department of Child Health, School of Medicine, Cardiff University, Heath Park, Cardiff CF14 4XN, UK
The impacts of hyper and hypothyroidism on body composition, i.e. the relative quantity and quality of bone,adipose tissue and muscle, have traditionally been attributed
uniquely to abnormal levels of free thyroid hormones. The presence of biologically active TSH receptors in bone, fat and muscle, raises the possibility that both thyroid hormones and TSH contribute to the changes in body composition associated with thyroid disease. Journal of Endocrinology (2010) 204, 13–20
Jeffrey Dach MD
7450 Griffin Road, Suite 190
Davie, Fl 33314
954-792-4663
http://www.bioidenticalhormones101.com/
http://www.jeffreydach.com
http://www.drdach.com
http://www.naturalmedicine101.com
http://www.truemedmd.com
Click Here for:Dr Dach’s Online Store for Pure Encapsulations Supplements
Click Here for:Dr Dach’s Online Store for Nature’s Sunshine Supplements
Web Site and Discussion Board Links:
http://jdach1.typepad.com/blog/
http://disc.yourwebapps.com/Indices/244124.html
http://disc.yourwebapps.com/Indices/244066.html
http://disc.yourwebapps.com/Indices/244067.html
http://disc.yourwebapps.com/Indices/244161.html
http://disc.yourwebapps.com/Indices/244163.html
Disclaimer click here: http://www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship. Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Link to this article: http://wp.me/P3gFbV-rO
http://jeffreydach.com/2011/05/06/why-natural-thyroid-is-better-than-synthroid-part-two-by-jeffrey-dach-md.aspx
Copyright (c) 2011-2014 Jeffrey Dach MD All Rights Reserved. This article may be reproduced on the internet without permission, provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.






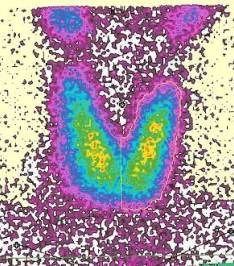



New Thyroid Book Stop the Thyroid Madness Two - Jeffrey Dach MD September 4, 2014 at 11:03 AM
[…] Natural Thyroid is Better Part Two […]