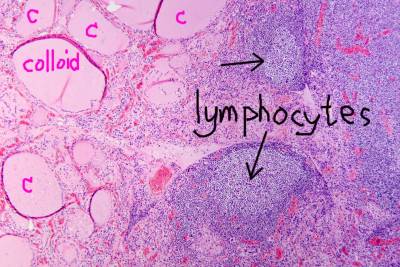
 Above image courtesy of wikimedia commons: Microscopy of thyroid gland showing normal structure on left (c=colloid follicles). Hashimoto’s thyroiditis seen on right, with lymphoid infiltration (black arrows). Autoantibodies against thyroid peroxidase and thyroglobulin were elevated.
Above image courtesy of wikimedia commons: Microscopy of thyroid gland showing normal structure on left (c=colloid follicles). Hashimoto’s thyroiditis seen on right, with lymphoid infiltration (black arrows). Autoantibodies against thyroid peroxidase and thyroglobulin were elevated.
Hashimotos Thyroiditis, Manic Depression, Psychosis and Psychiatric Manifestations by Jeffrey Dach MD
Pathophysiology of Hashimoto’s
Hashimoto’s thyroiditis is an autoimmune disease in which the thyroid gland is infiltrated by lymphocytes which attack and destroy the functioning thyroid cells called thyrocytes. These cells form a single layer lining the colloid follicles (see above image) storing the thyroglobulin colloid, the raw material precursor to thyroid hormone. The thyrocytes concentrate iodine from the blood stream, activate the iodine and combine it with thyroglobulin to form thyroid hormone (T4), which is then secreted into the blood stream.
Diagnostic Antibodies
Although the cellular infiltrate in the gland is the hallmark of the disease, the diagnosis of Hashimoto’s Thyroiditis is usually made by detection of anti-thyroid antibodies in the blood serum. These are the TPO (Thyroid Peroxidase) and Thyroglobulin Antibodies.
In addition, antibodies to the TSH Receptor consist of two types. TSH Blocking Antibodies cause hypothyroidism, while TSH Stimulating Antibodies cause hyperthyroidism. Other antibodies have also been detected against the NIS (sodium iodide symporter) and against Pendrin. (28) Future investigation may yet reveal additional antibodies currently unknown.
Clinical Course of Hashimoto’s Thyroiditis
The clinical course can be variable depending on severity of the inflammatory attack, and the amount of damaged thyroid tissue. Early on, Hashimoto’s has a 20-27%% chance of spontaneous recovery.(37)(33-40) Late stage disease is associated with hypothyroidism as the gland is usually destroyed and fibrotic.(28)
Thyroid Function May Vary – Hashi-Toxicosis
Thyroid function can be variable as well. Early stage disease may have normal thyroid function, or there may be episodic periods of transient hyperthyroidism, also called “Thyroid Storm” which if severe, may require hospitalization.
This hyperthyroidism of Hashimoto’s Disease has been named, “Hashitoxicosis”.(29-32) Indeed, thyroid function may fluctuate up and down. (36) The patient may cycle back and forth from low to high thyroid function which can mimic various psychiatric syndromes such as Bi-Polar Syndrome and Manic-Depressive Psychosis.(1-17)
Two explanations for Hashitoxicosis have been proposed.(28) One is that cell death of thyrocytes releases thyroid hormone into circulation producing transient thyroid storm. This is usually self limiting once the inflammatory attack and cell death of thyrocytes ceases.
The second explanation is that there may be alternating dominance of TSH Receptor Blocking Antibodies with TSH Receptor Stimulatory Antibodies. The TSH blocking antibodies cause hypothyroidism, while the TSH stimulating antibodies cause hyperthyroidism. Some Hashimoto’s patients will develop high TSH Receptor Antibody levels and transform into Graves Disease, a form of hyperthyroidism. Both Graves and Hashimoto’s may co-exist in the same patient and cause alternating episodes of hyper and hypo-thyroidism.(33-35)
 Psychiatric Manifestations of Hashimotos (1-27)
Psychiatric Manifestations of Hashimotos (1-27)
Various psychiatric syndromes have been associated with Hashimotos thyroiditis, including depression, anxiety, manic-depression, bipolar, acute psychosis, dementia, loss of cognitive function etc. (1-27) Most of these recover after treatment of Hashimototo’s thyroiditis with thyroid medication and other measures.
Left image Courtesy Wikimedia: Fear and anxiety.
Steroid Responsive Encehalopathy
However, a more severe form of neuro-psychiatric disturbance has been recently described called Hashimoto’s Encephalopathy. This may mimic the usual psychiatric disturbance, or may present as a more severe neurologic disorder with dementia, ataxia, seizures, epilepsy, cerebral vasculitis. Brain Perfusion Imaging and EEG studies may show abnormalities. (1-27)
Recognition of Hashimotos Encephalopathy is important because the disorder is exquisitely responsive to corticosteroid treatment with prompt remission in most cases. (1-27)
There is a high correlation between Hashimotos autoimmune thyroiditis and Celiac disease and other forms of Gluten Sensitivity. Indeed, in genetically predisposed indiviuals, gluten consumption may be associated with Gluten induced ataxia, encephalopathies, neuropsychiatric disorders, sensory neuropathies, cranial neuropathies, cerebral vasculitis etc., which may indeed overlap with the clinical presentation of Hashimotos encephalopathy. It would therefore be prudent for the Hashimotos patient to undergo testing for Celiac disease, and Gluten sensitivity the anti-gliadin antibody. Some practitioners advise a gluten free diet in spite of negative testing to guard against a false negative result.
Articles with Related Interest:
Iodine and Hashimotos Thyroiditis
Hashimotos Thyroid Disease and Molecular Mimicry
Selenium and the Thyroid More Good News
SSRI Drugs No Better Than Placebo
Jeffrey Dach MD
7450 Griffin Road, Suite 190
Davie, Fl 33314
954-792-4663
Links and references
Seizures and Psychosis
1) http://www.ncbi.nlm.nih.gov/
Korean J Pediatr. 2012 Mar;55(3):111-3.
A case of Hashimoto’s encephalopathy presenting with seizures and psychosis.Lee MJ, Lee HS, Hwang JS, Jung DE.
Hashimoto’s encephalopathy (HE) is a rare, poorly understood, autoimmune disease characterized by symptoms of acute or subacute encephalopathy associated with increased anti-thyroid antibody levels. Here, we report a case of a 14-year-old girl with HE and briefly review the literature. The patient presented with acute mental changes and seizures, but no evidence of infectious encephalitis. In the acute stage, the seizures did not respond to conventional antiepileptic drugs, including valproic acid, phenytoin, and topiramate. The clinical course was complicated by the development of acute psychosis, including bipolar mood, insomnia, agitation, and hallucinations. The diagnosis of HE was supported by positive results for antithyroperoxidase and antithyroglobulin antibodies. Treatment with methylprednisolone was effective; her psychosis improved and the number of seizures decreased. HE is a serious but curable, condition, which might be underdiagnosed if not suspected. Anti-thyroid antibodies must be measured for the diagnosis. HE should be considered in patients with diverse neuropsychiatric manifestations.
Manic Symptoms-response to steroids
2) http://neuro.psychiatryonline.
Manic Symptoms Associated With Hashimoto’s Encephalopathy: Response to Corticosteroid Treatment
Shuai-Ting Lin, M.D.; Cheng-Sheng Chen, M.D.; Pinchen Yang, M.D.; Cheng-Chung Chen, Ph.D. The Journal of Neuropsychiatry and Clinical Neurosciences 2011;23:E20-E21.
Manic-Psychosis and Brain Perfusion abnormalities
3) http://www.ncbi.nlm.nih.gov/
Clin Pract Epidemiol Ment Health. 2007 Dec 20;3:31.
Affective psychosis, Hashimoto’s thyroiditis, and brain perfusion abnormalities: case report.
Bocchetta A, Tamburini G, Cavolina P, Serra A, Loviselli A, Piga M.
It has recently become evident that circulating thyroid antibodies are found in excess among patients suffering from mood disorders. Moreover, a manic episode associated with Hashimoto’s thyroiditis has recently been reported as the first case of bipolar disorder due to Hashimoto’s encephalopathy. We report a case in which Hashimoto’s thyroiditis was suspected to be involved in the deteriorating course of mood disorder and discuss potential pathogenic mechanisms linking thyroid autoimmunity with psychopathology.
CASE PRESENTATION:A 43-year-old woman, with a history of recurrent depression since the age of 31, developed manic, psychotic, and soft neurological symptoms across the last three years in concomitance with her first diagnosis of Hashimoto’s thyroiditis. The patient underwent a thorough medical and neurological workup. Circulating thyroperoxidase antibodies were highly elevated but thyroid function was adequately maintained with L-thyroxine substitution. EEG was normal and no other signs of current CNS inflammation were evidenced. However, brain magnetic resonance imaging evidenced several non-active lesions in the white matter from both hemispheres, suggestive of a non-specific past vasculitis. Brain single-photon emission computed tomography showed cortical perfusion asymmetry particularly between frontal lobes.
CONCLUSION:We hypothesize that abnormalities in cortical perfusion might represent a pathogenic link between thyroid autoimmunity and mood disorders, and that the rare cases of severe Hashimoto’s encephalopathy presenting with mood disorder might be only the tip of an iceberg.
Acute Psychotic Epidodes
4) http://www.ncbi.nlm.nih.gov/
Psychosom Med. 2007 Feb-Mar;69(2):200-1.(free full text)
Psychiatric presentation of Hashimoto’s encephalopathy.
Arrojo M, Perez-Rodriguez MM, Mota M, Moreira R, Azevedo A, Oliveira A, Abreu P, Marques P, Silva A, Pereira JG, Palha AP, Baca-Garcia E.
Hashimoto’s encephalopathy is an unusual condition that is associated with Hashimoto’s thyroiditis. Myoclonus, epileptic seizures, dementia, and disturbances of consciousness are the most common features.
CASE REPORT:We present an atypical case of Hashimoto’s encephalopathy in a 33-year-old woman who presented with several brief and acute psychotic episodes. After treatment with steroids, there was an improvement in the patient’s psychiatric symptoms and electroencephalogram, and antithyroglobulin antibody titers returned to normal levels.
CONCLUSIONS:It is our opinion that Hashimoto’s encephalopathy should be considered in the differential diagnosis of atypical psychosis, especially because this is a treatable syndrome. This is particularly important in patients with a previous history of thyroid disease, despite current normal thyroid function.
Psychosis and EEG abnormalities – responds to steroids
5) http://www.ncbi.nlm.nih.gov/
Cogn Behav Neurol. 2007 Jun;20(2):138-40.
Psychosis and EEG abnormalities as manifestations of Hashimoto encephalopathy.
Sporis D, Habek M, Mubrin Z, Poljaković Z, Hajnsek S, Bence-Zigman Z.
Hashimoto encephalopathy (HE) is a distinct form of encephalopathy, which can manifest itself with purely psychiatric symptoms. A 38-year-old female with history of rheumatoid arthritis was treated with psychotropic drugs for a couple of years in psychiatric structures because of the onset of depressive symptoms, psychoticlike manifestations, and impairment of cognitive functions. The electroencephalography (EEG) was characterized by general slowing with high voltage (2 to 3 Hz) delta biphasic and triphasic waves. Once a firm diagnosis of HE was made, corticosteroid treatment resulted in resolution of her psychiatric symptoms, marked EEG improvement, and partial improvement in her cognitive functions. HE should be suspected in young females with history of autoimmune disorders and EEG abnormalities.
Presentile dementia improves with prednisone
6) http://www.ncbi.nlm.nih.gov/
East Asian Arch Psychiatry. 2011 Mar;21(1):32-6.
Presenile dementia: a case of Hashimoto’s encephalopathy.
Chong CS, Leung JL, Wong IH, Ng PW, Miao MY.
Hashimoto’s encephalopathy may present with a variety of neurological symptoms and signs, including myoclonus, epileptic seizures, disturbance of consciousness, psychosis, ataxia, and presenile dementia. This report is of a 57-year-old woman with a history of thyroid disease who was investigated for generalised seizures, rapid decline in cognitive function, increasing dependency, and gradual change in personality. High thyroid autoantibody titres confirmed the diagnosis of Hashimoto’s encephalopathy and her symptoms improved with treatment with prednisolone. The differential diagnosis of presenile dementia, aetiology and pathogenesis of Hashimoto’s encephalomyelitis, and treatment options are discussed. Hashimoto’s encephalomyelitis should be considered in the differential diagnosis of presenile dementia, particularly in patients with a history of thyroid disease.
Reversible dementia with psychosis-steroids
7) http://www.ncbi.nlm.nih.gov/pubmed/17109712
Psychiatry Clin Neurosci. 2006 Dec;60(6):761-3.
Reversible dementia with psychosis: Hashimoto’s encephalopathy.
Mocellin R, Lubman DI, Lloyd J, Tomlinson EB, Velakoulis D.
A case of presumed Hashimoto’s encephalopathy (HE) is presented. The presentation included memory loss, delusions, functional decline and culminated in a generalized seizure. Anti-thyroid antibodies were detected and symptoms resolved with prednisolone. Patients with HE may present with prominent neuropsychiatric symptoms, attract psychiatric diagnoses and present to psychiatric services. Primarily a diagnosis of exclusion, HE should be considered in cases of encephalopathy in which standard investigations are negative.
Reversible dementia and psychosis
8) http://www.ncbi.nlm.nih.gov/
Fortschr Neurol Psychiatr. 2008 Oct;76(10):610-5. doi: 10.1055/s-2008-1038253. Epub 2008 Oct 2.
[Hashimoto encephalopathy–a difficult differential diagnosis. A case report of reversible dementia and psychosis].
[Article in German] Nunnemann C, Kratz T.
Hashimoto encephalopathy is a rare disease that is associated with Hashimoto thyreoiditis. Dementia, disturbances of consciousness and epileptic seizures are the most common features.
CASE REPORT:We report a case of Hashimoto encephalopathy in a 74-year-old woman who presented with psychotic episodes, visual hallucinations, dementia, tremor, rigidity and fluctuation of consciousness. After treatment with steroids, cognitive function became normal and other symptoms improved significantly.
CONCLUSION:Hashimoto encephalopathy should be considered as a differential diagnosis of psychosis in combination with dementia and other neurological symptoms to dementia with Lewy bodies and Creutzfeldt-Jakob disease.
9) http://www.ncbi.nlm.nih.gov/
Psychosomatics. 1982 Apr;23(4):337-42.
Psychiatric manifestations of Hashimoto’s thyroiditis.
Hall RC, Popkin MK, DeVaul R, Hall AK, Gardner ER, Beresford TP.
10) http://journals.
J Neuropsychiatry Clin Neurosci. 2001 Fall;13(4):532-3.
Affective disorders associated with autoimmune thyroiditis.
Degner D, Meller J, Bleich S, Schlautmann V, Rüther E.
Acute Psychosis
11) http://www.ncbi.nlm.nih.gov/
Psychiatr Prax. 2003 May;30(Suppl 2):83-84.
[Acute Schizophrenic Disorder in a Patient with Hashimoto’s Thyroiditis] [Article in German] Teuber I, Volz HP.
While for some diseases with hyperthyreosis psychotic developments are well known, for a rare autoimmune thyroiditis, Hashimoto’s thyroiditis, only one case of development of psychotic symptoms is known. In this case-study we present a 42-year-old white female who was admitted to hospital showing symptoms of acute psychosis. The results of the laboratory examinations showed the constellation of beginning Hashimoto’s thyroiditis in hyperthyreotic state with high level of antithyroid peroxidase antibodies and comparatively low level of anti-TSH receptor antibodies. The patient recovered well in 4-weeks time under therapy with neuroleptics and benzodiazepines.
—————–
Hashimotos Encephalopathy
BMJ
13) http://www.ncbi.nlm.nih.gov/
http://www.ncbi.nlm.nih.gov/
BMJ Case Rep. 2010 Nov 23;2010. A series report of autoimmune hypothyroidism associated with Hashimoto’s encephalopathy: an under diagnosed clinical entity with good prognosis. Nayak HK, Daga MK, Kumar R, Garg SK, Kumar N, Mohanty PK.
Thyroid dysfunctions may be accompanied by numerous neurological and psychiatric disorders. The most well-known is cognitive impairment and depression in hypothyroid patients, as well as an increased risk of cerebrovascular accidents. A separate, although a rare entity, is Hashimoto’s encephalopathy. Unlike encephalopathy associated with other conditions, management in Hashimoto’s encephalopathy highly responds to steroid treatment and may be associated with normal thyroid profile at presentation. Hashimoto’s encephalopathy, while rare, may have been under-recognised since its clinical presentation overlaps several more common disorders, such as depression, seizures or anxiety. We present two cases of hypothyroidism with peculiar presentation. The first case has rapidly progressive neurological dysfunction, normal thyroid function at presentation, normal MRI finding and responds to steroid treatment. The second case has a subacute progressive neurological deterioration with elevated thyroid-stimulating hormone titre at presentation. Both these cases are known hypothyroidism on regular thyroxin replacement therapy with elevated anti-thyroid peroxidase antibodies. We conclude that Hashimoto’s encephalopathy can present with a wide spectrum of neurological illnesses in the setting of hypothyroidism. Thyroid status may vary from hypothyroid, normothyroid to even hyperthyroid. This condition usually has an abnormal electroencephalography (EEG) background and usually responds to high dose steroids.
When should the diagnosis of Hashimoto’s encephalopathy be entertained? Any neuropsychiatric condition that is not responding to conventional treatment, especially in the setting of probable or known autoimmune thyroiditis, should raise suspicion for Hashimoto’s encephalopathy.
14) http://www.ncbi.nlm.nih.gov/
Brain Nerve. 2013 Apr;65(4):365-76.
[Hashimoto’s encephalopathy and autoantibodies].
[Article in Japanese] Yoneda M.
Encephalopathy occasionally occurs in association with thyroid disorders, but most of these are treatable. These encephalopathies include a neuropsychiatric disorder associated with hypothyroidism, called myxedema encephalopathy. Moreover, Hashimoto’s encephalopathy (HE) has been recognized as a new clinical disease based on an autoimmune mechanism associated with Hashimoto’s thyroiditis. Steroid treatment was successfully administered to these patients.
Recently, we discovered that the serum autoantibodies against the NH2-terminal of α-enolase (NAE) are highly specific diagnostic biomarkers for HE.
Further, we analyzed serum anti-NAE autoantibodies and the clinical features in many cases of HE from institutions throughout Japan and other countries. Approximately half of assessed HE patients carry anti-NAE antibodies. The age was widely distributed with 2 peaks (20-30 years and 50-70 years). Most HE patients were in euthyroid states, and all patients had anti-thyroid (TG) antibodies and anti-thyroid peroxidase (TPO) antibodies. Anti-TSH receptor (TSH-R) antibodies were observed in some cases. The common neuropsychiatry features are consciousness disturbance and psychosis, followed by cognitive dysfunction, involuntary movements, seizures, and ataxia. Abnormalities on electroencephalography (EEG) and decreased cerebral blood flow on brain SPECT were common findings, whereas abnormal findings on brain magnetic resonance imaging (MRI) were rare. HE patients have various clinical phenotypes such as the acute encephalopathy form, the chronic psychiatric form, and other particular clinical forms, including limbic encephalitis, progressive cerebellar ataxia, and Creutzfeldt-Jakob disease (CJD)-like form. The cerebellar ataxic form of HE clinically mimics spinocerebellar degeneration (SCD) and is characterized by the absence of nystagmus, absent or mild cerebellar atrophy, and lazy background activities on EEG. Taken together, these data suggest that the possibility of encephalopathy associated with thyroid disorders must be considered.
15) http://www.ncbi.nlm.nih.gov/
J Neurol Neurosurg Psychiatry. 2007 February; 78(2): 196–197.
Hashimoto’s encephalopathy presenting with progressive cerebellar ataxia. H Nakagawa, M Yoneda, A Fujii, K Kinomoto, and M Kuriyama H Nakagawa, M Yoneda, A Fujii, K Kinomoto, M Kuriyama, Second Department of Internal Medicine, Faculty of Medical Sciences, University of Fukui, Fukui, Japan
Recently, we reported serum autoantibodies against the amino (NH2) terminal region of α enolase (NAE) as a useful diagnostic marker of Hashimoto’s encephalopathy
We describe here a patient with Hashimoto’s encephalopathy, who presented with progressive cerebellar ataxia with mild abnormality on electroencephalography (EEG) and showed marked improvement after steroid administration. The patient was diagnosed as having Hashimoto’s encephalopathy owing to the presence of the anti‐NAE antibodies as well as antithyroid antibodies in the serum.
16) http://www.ncbi.nlm.nih.gov/
Rinsho Byori. 2009 Mar;57(3):271-8.
[Anti-NAE autoantibodies and clinical spectrum in Hashimoto’s encephalopathy]. Matsunaga A, Yoneda M.
Hashimoto’s thyroiditis (HT) is the most common disorder affecting the thyroid gland. Encephalopathy associated with abnormal thyroid functions, such as myxedema encephalopathy, is treatable. Hashimoto’s encephalopathy (HE) was recognized as a new clinical disease based on an autoimmune mechanism associated with HT, and steroid treatment has been successfully administrated. Recently, we discovered serum autoantibodies against the NH2-terminal of a-enolase (NAE) as a specific diagnostic marker for HE. We analyzed these serum anti-NAE autoantibodies and the clinical features in 84 cases of HE. The 84 patients consisted of 26 men and 58 women, from many institutions throughout Japan and other countries. A total of 37 patients carried anti-NAE antibodies (44%). The age was widely distributed between 19 and 87 years old, with two peaks (around 20-30 and 50-70 years old). Most patients were in euthyroid states, and all patients had anti-thyroid (TG) and/or anti-thyroid peroxidase (TPO) antibodies, and anti-TSH receptor (TSHR) antibodies in some cases. Only 20% of patients had past histories of HT. The acute encephalopathy form was the most common clinical feature, and subacute or chronic psychiatric forms and other forms such as pure ataxia, limbic encephalopathy, and Creutzfeldt Jakob-like forms followed. The patients with anti NAE antibodies tended to exhibit acute encephalopathy. The most common neuropsychiatric features were consciousness disturbance, psychiatric symptoms, and seizures. Involuntary movements (tremor, myoclonus, or choreoathetosis) or ataxia occasionally occurred. Abnormalities, especially the slowing of background activities, on EEG and elevated levels of protein/IgG in cerebrospinal fluid (CSF) were common and useful laboratory findings for the diagnosis, while abnormalities on brain MRI were rare and non-specific in HE. Immunotherapies such as glucocorticoid, immunosuppressants, immunoglobulin, and plasma exchange, were recommended and effective for HE treatment. HE belongs to a part of a clinical spectrum consisting of individuals with anti-thyroid antibodies, overlapping the clinical spectrum of HT. Anti-NAE autoantibodies were positive in 44% of patients with HE. Considering the overall findings, we should be aware of the possibility of autoimmune encephalopathy associated with thyroid disorders (HE) in patients with an unknown etiology of neuronpsychiatric symptoms with/without a past history of HT.
17) http://www.ncbi.nlm.nih.gov/
J Neurol Neurosurg Psychiatry. 2001 Jul;71(1):81-7.
Ataxia associated with Hashimoto’s disease: progressive non-familial adult onset cerebellar degeneration with autoimmune thyroiditis. Selim M, Drachman DA. University of Massachusetts Medical School, 55 Lake Ave North, Worcester, MA 01655, USA.
18) http://www.ncbi.nlm.nih.gov/
Indian J Pediatr. 2007 May;74(5):492-4.
Hashimoto’s encephalopathy in an adolescent boy.
Ray M, Kothur K, Padhy SK, Saran P.
Hashimoto’s encephalopathy is an under-recognized cause of acute encephalopathy both in children and adults. We hereby describe a 12.5 yr old boy with this rare disorder that presented with an acute onset of episodic psychosis with hallucinations along with seizures and had elevated antithyroid antibodies. Symptoms improved with thyroxine replacement and anticonvulsants and EEG normalized 3 mth into follow up. Hashimoto’s encephalopathy should be considered in patients with unexplained encephalopathy and seizures, as prompt recognition and management can lead to an excellent outcome.
19) http://www.ncbi.nlm.nih.gov/
Pediatr Neurol. 2011 Dec;45(6):420-2.Hashimoto’s encephalopathy in children and adolescents.Erol I, Saygi S, Alehan F. Hashimoto’s encephalopathy is an underdiagnosed, steroid-responsive, progressive or relapsing encephalopathy associated with high titers of serum antithyroid antibodies. Although Hashimoto’s encephalopathy is well documented in adults, it is rarely observed or studied in children and adolescents. We describe the clinical and laboratory findings of four children (aged 9-15 years) with Hashimoto’s encephalopathy. The clinical features of two patients at presentation included epileptic seizures and confusion. The other presenting signs included breath-holding spells, behavioral problems, psychosis, and ataxia (one patient each). During their presentation, three patients were euthyroid, and one was hyperthyroid. All patients manifested increased antithyroid antibodies, and all improved with steroid treatment. Hashimoto’s encephalopathy is rarely suspected at presentation. Therefore, greater awareness of its signs by clinicians is necessary for proper diagnoses.
20) http://www.ncbi.nlm.nih.gov/
East Asian Arch Psychiatry. 2011 Mar;21(1):32-6. Presenile dementia: a case of Hashimoto’s encephalopathy. Chong CS, Leung JL, Wong IH, Ng PW, Miao MY. Hashimoto’s encephalopathy may present with a variety of neurological symptoms and signs, including myoclonus, epileptic seizures, disturbance of consciousness, psychosis, ataxia, and presenile dementia. This report is of a 57-year-old woman with a history of thyroid disease who was investigated for generalised seizures, rapid decline in cognitive function, increasing dependency, and gradual change in personality. High thyroid autoantibody titres confirmed the diagnosis of Hashimoto’s encephalopathy and her symptoms improved with treatment with prednisolone. The differential diagnosis of presenile dementia, aetiology and pathogenesis of Hashimoto’s encephalomyelitis, and treatment options are discussed. Hashimoto’s encephalomyelitis should be considered in the differential diagnosis of presenile dementia, particularly in patients with a history of thyroid disease.
21) http://www.ncbi.nlm.nih.gov/
Rinsho Shinkeigaku. 2002 Feb;42(2):162-6.Hashimoto’s encephalopathy–case report and diagnostic issues in Japan]. [Article in Japanese] Nakamura H, Tokonami F, Yamasaki M.
Epileptic Disord. 2011 Sep;13(3):253-8. Non-convulsive status epilepticus of frontal origin as the first manifestation of Hashimoto’s encephalopathy. Monti G, Pugnaghi M, Ariatti A, Mirandola L, Giovannini G, Scacchetti S, Nichelli P, Meletti S.Hashimoto’s encephalopathy is an often misdiagnosed, life threatening, condition which improves promptly with steroid therapy. Since clinical manifestations are heterogeneous and non-specific, the diagnosis is often difficult. Several case reports of Hashimoto’s encephalopathy presenting with partial or generalised seizures are described, but only a few have focused on status epilepticus as the first clinical manifestation. We report two patients presenting with repetitive and prolonged seizures characterised by progressive reduction in contact and reactivity associated with frontal/diffuse polyspike-and-wave activities. This condition, which can be interpreted as a form of non-convulsive status epilepticus (NCSE) of frontal origin, was refractory to antiepileptic drugs but responded promptly to high doses of intravenous steroid treatment. In cases of unexplained encephalopathy with EEG documentation of NCSE, the early recognition and treatment of Hashimoto’s encephalopathy may lead to a favourable prognosis. [Published with video sequences].
23) http://www.ncbi.nlm.nih.gov/
Wilcox RA, To T, Koukourou A, Frasca J.Hashimoto’s encephalopathy (HE) is a relapsing, but exquisitely corticosteroid-responsive encephalopathy associated with autoimmune thyroiditis. Although a rare disease, with just over 100 cases reported, it may be under-recognised. Its presentation can be protean with prominent neuropsychiatric features, stroke-like episodes, seizures and myoclonic jerks. Prompt corticosteroid treatment usually leads to rapid recovery. Here we report a patient with HE, initially presenting with florid neuropsychiatric symptoms. Recent developments in the understanding of this condition are discussed.
Srp Arh Celok Lek. 2005 Oct;133 Suppl 1:88-91.
[Autoimmune thyroid disease and brain]. [Article in Serbian] Zarković M.
Changes of the affective and cognitive function are usually associated with thyroid gland dysfunction. In autoimmune thyroid disease, these changes can be caused by thyroid dysfunction (hypo- or hyperthyroidism) or associated with the presence of antithyroid antibodies. Even a small change in thyroid hormone concentration is associated with change of cognitive function. In euthyroid older males, variation of total and free thyroxin accounts for about 10% of Wechsler adult intelligence test variance. In euthyroid females, lower cognitive function, measured by Mini Mental test, also correlates with blood thyroxin. Short-term (4 weeks) hypothyroidism induces clinically significant cognitive dysfunction, which is reversible by thyroid hormone substitution. Mild hypothyroidism (TSH less than 10) also induces reversible cognitive dysfunction. In hypothyroidism, PET scanning shows global reduction of brain blood flow and glucose metabolism. Hashimoto’s encephalopathy is characterized by corticosteroid reversible encephalopathy associated with the presence of antithyroid antibodies. Encephalopathy can be manifested as multiple stroke-like episodes (vasculitis like), or as diffuse, progressive type characterized by dementia and psychiatric symptoms. In euthyroid patients with Hashimoto’s thyroiditis and no evidence of neurological disease, SPECT showed brain perfusion abnormalities. Post mortem and brain biopsy findings can be normal or show perivascular lymphocytic infiltration. Recently, presence of antineuronal antibodies has been found in patients with Hashimoto’s thyroiditis. Specific high reactivity against human alpha-enolase was high in patients with Hashimoto’s encephalopathy, but absent in patients with other neurological disorders and healthy subjects. Specific antineural antibodies were found in another group of Hashimoto’s encephalopathy patients. Furthermore, Ferracci et al, found antithyroid antibodies in the CSF of patients with Hashimoto’s encephalopathy.
25) http://www.ncbi.nlm.nih.gov/
26) http://www.ncbi.nlm.nih.gov/
Intern Emerg Med. 2006;1(1):15-23. Clinical and diagnostic aspects of encephalopathy associated with autoimmune thyroid disease (or Hashimoto’s encephalopathy). Tamagno G, Federspil G, Murialdo G.Encephalopathy associated with autoimmune thyroid disease, currently known as Hashimoto’s encephalopathy, but also defined as corticosteroid-responsive encephalopathy associated with autoimmune thyroiditis, is a relatively rare condition observed in a small percentage of patients presenting with autoimmune thyroid disease. It consists of a subacute, relapsing-remitting, steroid-responsive encephalopathy characterised by protean neurologic and neuropsychiatric symptoms, diffuse electroencephalographic abnormalities and increased titres of antithyroid antibodies in serum and/or in cerebrospinal fluid. Most of the cases presenting this neurologic complication are affected by Hashimoto’s thyroiditis or, less frequently, by other autoimmune thyroid diseases, chiefly Graves’ disease. The pathogenesis of this encephalopathy is still unknown and largely debated, because of extremely varied clinical presentation, possibly referable to different aetiologic and pathophysiologic mechanisms, as confirmed by the two clinical cases we report in this paper. Autoimmune aetiology is, however, very likely in view of the well established favourable response to corticosteroid administration. Both vasculitis and autoimmunity directed against common brain-thyroid antigens represent the most probable aetiologic pathways. Clinical manifestations include consciousness changes, neurologic diffuse or focal signs, headache, and altered cognitive function. Although unspecific, cerebral oedema has also been described. Cerebrospinal fluid examination often discloses an inflammatory process, with a mild increase in protein content and occasionally in lymphocyte count. In this review, clinical criteria for the diagnosis of defined, probable, or possible encephalopathy associated with autoimmune thyroid disease are suggested. Corticosteroid therapy currently allows us to obtain rapid remission of disease symptoms, but adverse outcomes as well as spontaneous remissions have also been reported.21)
27) http://www.ncbi.nlm.nih.gov/
Best Pract Res Clin Endocrinol Metab. 2005 Mar;19(1):53-66.
Hashimoto’s encephalopathy: myth or reality? An endocrinologist’s perspective. Fatourechi V.
Since the first description of a case of episodic encephalopathy associated with Hashimoto’s thyroiditis in 1966, many cases of corticosteroid-responsive encephalopathy associated with positive antithyroid antibodies, clinical Hashimoto’s thyroiditis, or spontaneous autoimmune thyroid failure have been reported. These patients have neurologic manifestations of encephalopathy unrelated to other known causes. The condition has thus been termed ‘Hashimoto’s encephalopathy’. The literature shows no proven association between thyroid disease and the neurologic process. Although the association of a common endocrinologic condition and a rare neurologic disease may occur by chance, this type of encephalopathy probably has an autoimmune nature and thus is more likely to occur in the background of another autoimmune condition such as autoimmune thyroid disease. Until the pathogenesis of these coincident conditions is better defined, the term ‘corticosteroid-responsive encephalopathy associated with autoimmune thyroiditis’ is more accurate and descriptive than Hashimoto’s encephalopathy. Advances in the field may clarify this seemingly inconsistent terminology.
28) http://www.thyroidmanager.org/chapter/hashimotos-thyroiditis/
Hashimoto’s Thyroiditis Last Updated: December 20, 2013 Takashi Akamizu, M.D., Ph.D. , Nobuyuki Amino, M.D. Leslie J. DeGroot, M.D.
Hashitoxicosis
29) http://www.thetrp.net/text.asp?2013/10/4/5/106803
Unnikrishnan A G. Hashitoxicosis: A clinical perspective.
Thyroid Res Pract [serial online] 2013 [cited 2014 Feb 8];10:5-6.
AG Unnikrishnan Department of Endocrinology, Amrita Institute of Medical Sciences, Cochin, Kerala, India
Date of Web Publication 2-Feb-2013
30) http://www.touchendocrinology.com/articles/hashitoxicosis-three-cases-and-review-literature
http://www.touchbriefings.com/pdf/3186/strobel.pdf.
Harsch IA, Hahn EG, Strobel D.
Hashitoxicosis – Three cases and a review of the literature. Touch Briefings (European Endocrinology) 2008. p. 70-2.
[Last accessed on 2012 Jan 9].
31) http://www.ncbi.nlm.nih.gov/pubmed/22286076
Horm Res Paediatr. 2012;77(1):36-40. doi: 10.1159/000334640. Epub 2012 Jan 26. Outcomes of children with hashitoxicosis. Wasniewska M, Corrias A, Salerno M, Lombardo F, Aversa T, Mussa A, Capalbo D, De Luca F, Valenzise M.
To investigate hashitoxicosis outcome in 14 children with persistent absence of thyrotropin receptor autoantibodies who were followed for 1.3-8.8 years (mean 3.5 ± 2.5). Due to a more severe presentation, 4 patients required methimazole (subgroup A1), whilst in the remaining 10 cas es (subgroup A2) no treatment was given.
RESULTS:A definitive resolution of hyperthyroidism was recorded 8.3 ± 6.3 months after diagnosis, even though there was a wide variability between subjects (3-23 months). In subgroup A2, hyperthyroidism resolution occurred spontaneously and earlier with respect to subgroup A1 (4.8 ± 2.0 months after diagnosis vs. 17.0 ± 4.5, p = 0.00001). After hyperthyroidism resolution, no relapses were recorded in any patients. Hyperthyroidism duration positively correlated with thyroid peroxidase autoantibody (TPOAb) levels at presentation (r = 0.729, p = 0.002).
CONCLUSIONS:In all the 14 hashitoxicosis children with persistently absent thyrotropin receptor autoantibodies, the hyperthyroid phase was widely variable and always followed by definitive resolution with no relapses and persistent euthyroidism or hypothyroidism. In the few patients with a more severe presentation, methimazole treatment was required, and definitive hyperthyroidism resolution was delayed. In this subgroup, TPOAb levels at diagnosis were higher than in the subgroup with less severe presentation and earlier hyperthyroidism resolution, suggesting a relationship between TPOAb levels and severity of the disease.
TSI test may be negative in 50% of children with Graves
32) http://www.ncbi.nlm.nih.gov/pubmed/19189704
J Pediatr Endocrinol Metab. 2008 Nov;21(11):1085-8.
Thyroid stimulating immunoglobulin is often negative in children with Graves’ disease. Rahhal SN, Eugster EA.
The diagnosis of Graves’ disease (GD) is typically confirmed with a thyroid stimulating immunoglobulin (TSI) titer. While TSI is reported to be positive in >90% of patients with GD, our anecdotal experience suggests that TSI negative GD may be more common in children.
AIM: To investigate the incidence of TSI negative GD in our population and to compare patients with TSI negative vs TSI positive GD.
METHODS: Charts of children with GD seen in our pediatric endocrinology clinic over the past 5 years were reviewed.
RESULTS: Fifty-seven patients with GD were included. TSI was negative in 43% of patients. No significant differences were found in children with TSI negative vs TSI positive GD.
CONCLUSIONS: In patients with GD, the finding of a negative TSI titer usually creates diagnostic uncertainty. However, the fact that nearly half of our patients with GD were TSI negative suggests that this is common in children.
spontaneous reversal of autoimmune hypothyroidism
33) http://www.ijpeonline.com/content/2012/1/9
Case report: rapid spontaneous recovery from severe hypothyroidism in 2 teenage girls. Paul B Kaplowitz Division of Endocrinology, Children’s National Medical Center, 111 Michigan Ave NW, Washington, 20010, DC, USA
Pediatrics, George Washington University School of Medicine and the Health Sciences, Washington, DC, USA
International Journal of Pediatric Endocrinology 2012, 2012:9
34) http://www.ncbi.nlm.nih.gov/pubmed/1732791
N Engl J Med. 1992 Feb 20;326(8):513-8. (free full text)
Disappearance of thyrotropin-blocking antibodies and spontaneous recovery from hypothyroidism in autoimmune thyroiditis.
Takasu N, Yamada T, Takasu M, Komiya I, Nagasawa Y, Asawa T, Shinoda T, Aizawa T, Koizumi Y.
Hypothyroidism may result from the production of antibodies that block the actions of thyrotropin. How often these thyrotropin-blocking antibodies are a cause of hypothyroidism and whether their production may cease, causing hypothyroidism to disappear, have not been extensively studied.
METHODS:We determined the frequency with which thyrotropin-blocking antibodies were present in 172 hypothyroid patients with goitrous autoimmune thyroiditis (Hashimoto’s disease) and 64 hypothyroid patients with atrophic autoimmune thyroiditis (idiopathic primary hypothyroidism). For 6 to 11 years we then followed 21 of these patients who were found to have thyrotropin-blocking antibodies. They received levothyroxine therapy for 3.5 to 8 years, after which it was discontinued. At frequent intervals during this time we measured the patients’ serum concentrations of thyroxine, triiodothyronine, thyrotropin, and thyrotropin-blocking antibodies (measured as immunoglobulins that inhibit thyrotropin binding and immunoglobulins that inhibit thyrotropin bioactivity).
RESULTS:Thyrotropin-blocking antibodies were detected in 9 percent of the patients with goitrous autoimmune thyroiditis and in 25 percent of those with atrophic autoimmune thyroiditis. Among the 21 patients studied serially while receiving levothyroxine, thyrotropin-blocking antibodies disappeared in 15 (group 1), 7 of whom had goiter initially, and persisted in 6 (group 2), none of whom had goiter initially. Levothyroxine therapy was subsequently discontinued in these 21 patients. Six of those in group 1 (four with goiter) remained euthyroid (mean follow-up after discontinuation of therapy, 2.1 years), and nine became hypothyroid again within 3 months. All six patients in group 2 remained hypothyroid.
CONCLUSIONS:Hypothyroidism in some patients with autoimmune thyroiditis may be due to thyrotropin-blocking antibodies. The production of thyrotropin-blocking antibodies may subside, producing remissions of hypothyroidism. Chronic autoimmune thyroiditis may therefore cause transient as well as permanent hypothyroidism.
35) http://www.ncbi.nlm.nih.gov/pubmed/22655217 free full text
J Thyroid Res. 2012;2012:182176. doi: 10.1155/2012/182176. Epub 2012 May 10.
Changes of TSH-Stimulation Blocking Antibody (TSBAb) and Thyroid Stimulating Antibody (TSAb) Over 10 Years in 34 TSBAb-Positive Patients with Hypothyroidism and in 98 TSAb-Positive Graves’ Patients with Hyperthyroidism: Reevaluation of TSBAb and TSAb in TSH-Receptor-Antibody (TRAb)-Positive Patients.
Takasu N, Matsushita M.
TWO TRABS: TSBAb and TSAb. TSBAb causes hypothyroidism. TSAb causes Graves’ hyperthyroidism. TSBAb and TSAb block TSH-binding to cells as TRAb, measured as TSH-binding inhibitory immunoglobulin (TBII). We reevaluate TSBAb and TSAb. We studied TSBAb, TSAb, and TBII over 10 years in 34 TSBAb-positives with hypothyroidism and in 98 TSAb-positives with hyperthyroidism. Half of the 34 TSBAb-positives with hypothyroidism continued to have persistently positive TSBAb, continued to have hypothyroidism, and did not recover from hypothyroidism. Ten of the 98 TSAb-positives with hyperthyroidism continued to have positive TSAb and continued to have hyperthyroidism. TSBAb had disappeared in 15 of the 34 TSBAb-positives with hypothyroidism. With the disappearance of TSBAb, recovery from hypothyroidism was noted in 13 (87%) of the 15 patients. TSAb had disappeared in 73 of the 98 TSAb-positives with hyperthyroidism. With the disappearance of TSAb, remissions of hyperthyroidism were noted in 60 (82%) of the 73. Two of the 34 TSBAb-positives with hypothyroidism developed TSAb-positive Graves’ hyperthyroidism. Two of the 98 TSAb-positive Graves’ patients with hyperthyroidism developed TSBAb-positive hypothyroidism. TSBAb and TSAb are TRAbs. TSBAb-hypothyroidism and TSAb-hyperthyroidism may be two aspects of one disease (TRAb disease). Two forms of autoimmune thyroiditis: atrophic and goitrous. We followed 34 TSBAb-positive patients with hypothyroidism (24 atrophic and 10 goitrous) over 10 years. All of the 10 TSBAb-positive goitrous patients recovered from hypothyroidism and 19 (79%) of the 24 TSBAb-positive atrophic patients continued to have hypothyroidism.
Alternating hyper and hypo case report
36) http://www.plosmedicine.org/article/info%3Adoi%2F10.1371%2Fjournal.pmed.0020089
Alzahrani AS, Aldasouqi S, Abdel Salam S, Sultan A (2005) Autoimmune Thyroid Disease with Fluctuating Thyroid Function. PLoS Med 2(5): e89. doi:10.1371/journal.pmed.0020089
Presentation of Case – A 38-y-old East Asian woman presented in 1985 with weight gain and cold intolerance. She was found to have a small goiter and an elevated thyroid-stimulating hormone (TSH) level of 58 mU/l (normal range, 0.5–5). She was diagnosed with primary hypothyroidism and was treated with levothyroxine (L-T4) 0.1 mg/d. Her symptoms promptly improved. Between 1985 and 1993, she felt generally well. Her adherence to treatment was variable, and when she was reviewed her TSH levels were raised on several occasions (in the range of 15–38 mU/l). In her past medical history, she had an ectopic pregnancy in 1990 and bilateral oophorectomy in 2000 for benign cystadenomas. There was no family history of thyroid or autoimmune diseases.
normally 27 % recovery over time from HASHIMOTOS
37) http://www.ncbi.nlm.nih.gov/pubmed/1951380
Am J Med. 1991 Oct;91(4):363-70.
Natural history of thyroid abnormalities: prevalence, incidence, and regression of thyroid diseases in adolescents and young adults.
Rallison ML, Dobyns BM, Meikle AW, Bishop M, Lyon JL, Stevens W.
This study reports the prevalence, incidence, and regression of thyroid abnormalities in a population observed from adolescence to adulthood.
PATIENTS AND METHODS: Examinations for thyroid abnormalities were performed in 4,819 school-age children, ages 11 to 18, in 1965 to 1968; two thirds of this original cohort (3,121) were re-examined 20 years later (1985 to 1986). Each subject with a thyroid abnormality detected by physical examination was studied by means of a series of re-examinations, and tests of thyroid function, imaging, and biopsy to determine the exact nature of the thyroid abnormality.
RESULTS: In the initial examinations (1965 to 1968), 185 thyroid abnormalities were found (3.7%). Diffuse hypertrophy with normal function (adolescent goiter) was the most common abnormality (19.3/1,000); 12.7/1,000 had chronic lymphocytic thyroiditis, and 4.6/1,000 had thyroid nodules, including two papillary carcinomas. Hyperthyroidism or hypothyroidism was found in 1.9/1,000. In the follow-up examinations in 1985 to 1986, 298 subjects had thyroid abnormalities (10.5%), of whom 81 (28.7/1,000) had simple goiters, 145 (51.3/1,000) had chronic thyroiditis, 45 (15.9/1,000) had hypothyroidism, 11 (3.9/1,000) had hyperthyroidism, and 66 (23.2/1,000) had nodules, which included 10 carcinomas. Of the 92 subjects with simple or adolescent goiter in 1965 to 1968, 60% were normal by 1985 to 1986, 20% were unchanged, and a few had developed thyroiditis (10%) or colloid goiters (3.0%). Of 61 subjects with thyroiditis, 27% had become normal, 33% remained unchanged, and 33% had become hypothyroid. Of the 22 subjects with thyroid nodules, two had complete disappearance of the nodules, and three had nodules considered to be variants of normal. The others exhibited a variety of nodular pathologic conditions.
CONCLUSIONS: The natural history of thyroid disorders, including simple goiter, chronic thyroiditis, hyperthyroidism, hypothyroidism, and nodular diseases of the thyroid, indicates they are dynamic and changeable in form, function, appearance, and disappearance.
spontaneous recovery from HASHIMOTOS
38) http://www.ncbi.nlm.nih.gov/pubmed/6687775
Acta Endocrinol (Copenh). 1983 Apr;102(4):531-4.
Recovery of thyroid function with a decreased titre of antimicrosomal antibody in a hypothyroid man with Hashimoto’s thyroiditis. Yamamoto M, Kaise K, Kitaoka H, Yoshida K, Kaise N, Fukazawa H, Sakurada T, Saito S, Yoshinaga K.
Abstract A 36 year old man with a diffuse goitre, signs of mild hypothyroidism, strikingly low levels of T4 (0.9 micrograms/dl) and T3 (24 ng/dl), elevated TSH (140 microU/ml) and elevated microsomal haemagglutination antibody (MCHA, 1:409 600), subsequently became non-goitrous and euthyroid with a decreased titre of antimicrosomal antibody without any medication. At the time of surgical biopsy, serum levels of T4 and T3 had risen to the normal range (4.6 micrograms/dl and 73 ng/dl, respectively), serum TSH had decreased to 30 microU/ml and the titre of MCHA to 1:25 600. Thyroid specimens showed Hashimoto’s thyroiditis. The activity of thyroid peroxidase (TPO) was normal. The latest examination, 1 year and 3 months after initial evaluation, showed that the patient remained euthyroid with no goitre, that serum thyroid hormones were within the normal range (T4 7.7 micrograms/dl and T3 97 ng/dl), and that TSH was not detectable. The titre of MCHA decreased strikingly to 1:400.
TSH blocking antibodies
39) http://www.ncbi.nlm.nih.gov/pubmed/1732791
N Engl J Med. 1992 Feb 20;326(8):513-8.
Disappearance of thyrotropin-blocking antibodies and spontaneous recovery from hypothyroidism in autoimmune thyroiditis.
Takasu N, Yamada T, Takasu M, Komiya I, Nagasawa Y, Asawa T, Shinoda T, Aizawa T, Koizumi Y.
Hypothyroidism may result from the production of antibodies that block the actions of thyrotropin. How often these thyrotropin-blocking antibodies are a cause of hypothyroidism and whether their production may cease, causing hypothyroidism to disappear, have not been extensively studied.
METHODS:We determined the frequency with which thyrotropin-blocking antibodies were present in 172 hypothyroid patients with goitrous autoimmune thyroiditis (Hashimoto’s disease) and 64 hypothyroid patients with atrophic autoimmune thyroiditis (idiopathic primary hypothyroidism). For 6 to 11 years we then followed 21 of these patients who were found to have thyrotropin-blocking antibodies. They received levothyroxine therapy for 3.5 to 8 years, after which it was discontinued. At frequent intervals during this time we measured the patients’ serum concentrations of thyroxine, triiodothyronine, thyrotropin, and thyrotropin-blocking antibodies (measured as immunoglobulins that inhibit thyrotropin binding and immunoglobulins that inhibit thyrotropin bioactivity).
RESULTS:Thyrotropin-blocking antibodies were detected in 9 percent of the patients with goitrous autoimmune thyroiditis and in 25 percent of those with atrophic autoimmune thyroiditis. Among the 21 patients studied serially while receiving levothyroxine, thyrotropin-blocking antibodies disappeared in 15 (group 1), 7 of whom had goiter initially, and persisted in 6 (group 2), none of whom had goiter initially. Levothyroxine therapy was subsequently discontinued in these 21 patients. Six of those in group 1 (four with goiter) remained euthyroid (mean follow-up after discontinuation of therapy, 2.1 years), and nine became hypothyroid again within 3 months. All six patients in group 2 remained hypothyroid.
CONCLUSIONS:Hypothyroidism in some patients with autoimmune thyroiditis may be due to thyrotropin-blocking antibodies. The production of thyrotropin-blocking antibodies may subside, producing remissions of hypothyroidism. Chronic autoimmune thyroiditis may therefore cause transient as well as permanent hypothyroidism.
40) http://www.ijpeonline.com/content/2012/1/9
Case report: rapid spontaneous recovery from severe hypothyroidism in 2 teenage girls. Paul B Kaplowitz Division of Endocrinology, Children’s National Medical Center, 111 Michigan Ave NW, Washington, 20010, DC, USA International Journal of Pediatric Endocrinology 2012,
Link to this page: http://wp.me/p3gFbV-1fq
Jeffrey Dach MD
7450 Griffin Road, Suite 190
Davie, Fl 33314
954-792-4663
www.jeffreydach.com
www.drdach.com
www.naturalmedicine101.com
www.bioidenticalhormones101.com
www.truemedmd.com
Click Here for: Dr Dach’s Online Store for Pure Encapsulations Supplements
Click Here for: Dr Dach’s Online Store for Nature’s Sunshine Supplements
Web Site and Discussion Board Links:
jdach1.typepad.com/blog/
disc.yourwebapps.com/Indices/244124.html
disc.yourwebapps.com/Indices/244066.html
disc.yourwebapps.com/Indices/244067.html
disc.yourwebapps.com/Indices/244161.html
disc.yourwebapps.com/Indices/244163.html
Disclaimer click here: www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship. Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Link to this page: http://wp.me/p3gFbV-1fq
Copyright (c) 2014 Jeffrey Dach MD All Rights Reserved. This article may be reproduced on the internet without permission, provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.










Production of Thyroid Hormone - Jeffrey Dach MD February 17, 2014 at 8:23 AM
[…] Hashimotos Thyroiditis, Manic Depression, Psychosis and Psychiatric Manifestations […]
The Use of Iodine in Graves Hyperthyroidism April 7, 2014 at 9:54 AM
[…] Hashimotos Thyroiditis, Manic Depression, Psychosis and Psychiatric Manifestations […]
B12 Deficiency and Neuro-Psychiatric Disorders by Jeffrey Dach MD - Jeffrey Dach MD April 24, 2014 at 9:29 AM
[…] Hashimoto’s thyroiditis which can mimic a manic-depressive disorder. See my previous article on […]
Myo-Inositol for PCOS and Hashimotos - Jeffrey Dach MD June 18, 2014 at 1:47 PM
[…] Hashimotos Part Three […]