 A Man with MDD Major Depressive Disorder Caused by Leaky Gut
A Man with MDD Major Depressive Disorder Caused by Leaky Gut By Jeffrey Dach MD
A 52 year old male came to see me in the office. He is a successful business man with a string of lucrative stores. He is currently under the care of a psychiatrist who prescribes two different anti-depressant drugs for chronic depression, an SSRI drug and Lithium Carbonate. In spite of the medications, the patient complains of continued symptoms of depression, chronic fatigue, vague body aches and pains and arthritis.
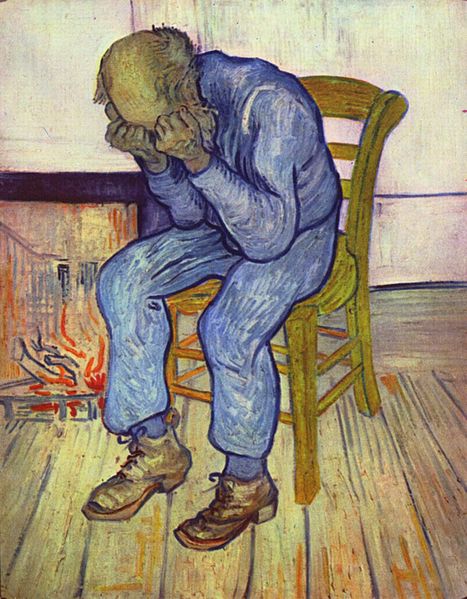
Upper left image: Painting by Vincent van Gogh (1853–1890) entitled “At Eternity’s Gate” May 1890, oil on canvas in the Kröller-Müller Museum. Courtesy of wikimedia commons.
The patient also complains of abdominal gas and bloating, especially after meals. Laboratory studies showed a low testosterone level of 267 (Total Testosterone). His Enterolabs stool antigliadin IgA antibody was markedly elevated (90 with normal less than 10). His Enterolabs panel also showed multiple food sensitivities. This was strongly suggestive of “Leaky Gut ” originating from wheat gluten sensitivity, along with other food intolerances. He was immediately started on Testosterone supplementation and a Gluten free diet, and noted improvement in symptoms. The patient was able to taper off one of the antidepressant meds (the Lithium) and reduced the SSRI drug dosage. A calcium score test was done showing a high calcium score of 490 (95th percentile) indicating high risk for underlying coronary artery disease, and the patient’s cardiologist started him on a statin anti-cholesterol drug (Crestor).
My previous article discussed how Gluten Sensitivity causes opening of the Tight Junctions in the GI mucosa, leading to leaky gut, and through “molecular mimicry” various autoimmune diseases. This same “Leaky Gut” mechanism may cause MDD (Major Depressive Disorder). This has been elucidated by Michael Maes MD PhD in many studies published over the last decade, showing that inflammation is the real etiology of depression. (1-6)(9-16)
The leaky gut, according to Dr Michael Maes causes inflammation in the brain causing depression, and may also cause inflammation in other organ systems such as the coronary arteries leading to elevated calcium score from underlying coronary artery disease.
The “leakage” of LPS (Lipo Poly Saccharide bacterial antigens) into the blood stream evokes activation of the innate immune system, and inflammation in the body and the brain and has been directly implicated as a cause of MDD (major depressive disorder). Dr Maes reports in an elegant study elevated IgM and IgG antibodies to LPS in both Depression and Chronic Fatigue. As patients are treated and the Leaky Gut Heals, symptoms improve over time, and the antibody titers decline(link to article).(1-6)(9-16)
Upper left image: SSRI antidepressant pills don’t help with “Leaky Gut Syndrome”. Courtesy of wikimedia commons.
A useful medical tool for chronic fatigue and chronic depression is the ALCAT test which measures white blood cell activation by food or environmental chemicals. Leaky gut allows not only bacterial LPS to leak, it also allows food particles to leak into the blood stream which may then activate the immune system. The ALCAT test is an elegant method to identify which foods or chemicals are causing the problem. Once this information is known, and the diet modified to eliminate the offending foods, immune acitivation and inflammatory response in the body is reduced to low levels with resolution of the fatigue and depression.
Since the depression and chronic fatigue is directly caused by the “Leaky Gut”. healing the leaky gut is the most direct way to make the patient better. There are a number of protocols for healing the leaky gut.
Secondly, identifying foods and environmental chemicals that are activating the white blood cells (the innate imune system, the ALCAT test) is extremely beneficial.
Thirdly, supplements to heal the gut such as Glutamine, GI Fortify and GI Integrity are very useful.
Fourthly, a program from BioBotanical Reseach using anti-microbial botanicals called Biocidin and Olivirex, Proflora (probiotic) are very useful.
Drugs handed out by the mainstream medical system are unhelpful when the underlying etiology is a “Leaky Gut”. Taking an SSRI antidepressant drug does nothing to ameliorate the Leaky Gut, immune activation, and inflammation in the patient with Major Depressive Disorder or Chronic Fatigue. Same can be said for other psychoactive drugs such as benzodiazepines, sleeping pills, amphetamines and narcotics which are handed out rather freely to many of these patients, causing more harm than good.
If Major Depressive Disorder is caused by inflammation related to “Leaky Gut Syndrome”, as proposed by Dr Michael Maes and others, then SSRI drugs and other Psycho-Active drugs should not be expected to resolve the issue, and probably cause more harm than good.
Articles with Related Interest:
Jeffrey Dach MD
7450 Griffin Road Suite 190
Davie, FL 33314
954-792-4663
Links and References
2007 Chronic Fatigue Syndrome
1) www.ncbi.nlm.nih.gov/pubmed/17007934
http://www.cfids-cab.org/rc/Maes.pdf
J Affect Disord. 2007 Apr;99(1-3):237-40. Epub 2006 Sep 27.
Increased serum IgA and IgM against LPS of enterobacteria in chronic fatigue syndrome (CFS): indication for the involvement of gram-negative enterobacteria in the etiology of CFS and for the presence of an increased gut-intestinal permeability.
Maes M, Mihaylova I, Leunis JC. Source MCare4U Outpatient Clinics, Antwerp, Belgium.
Abstract There is now evidence that chronic fatigue syndrome (CFS) is accompanied by immune disorders and by increased oxidative stress. The present study has been designed in order to examine the serum concentrations of IgA and IgM to LPS of gram-negative enterobacteria, i.e. Hafnia alvei; Pseudomonas aeruginosa, Morganella morganii, Proteus mirabilis, Pseudomonas putida, Citrobacter koseri, and Klebsiella pneumoniae in CFS patients, patients with partial CFS and normal controls. We found that the prevalences and median values for serum IgA against the LPS of enterobacteria are significantly greater in patients with CFS than in normal volunteers and patients with partial CFS. Serum IgA levels were significantly correlated to the severity of illness, as measured by the FibroFatigue scale and to symptoms, such as irritable bowel, muscular tension, fatigue, concentration difficulties, and failing memory. The results show that enterobacteria are involved in the etiology of CFS and that an increased gut-intestinal permeability has caused an immune response to the LPS of gram-negative enterobacteria. It is suggested that all patients with CFS should be checked by means of the IgA panel used in the present study and accordingly should be treated for increased gut permeability.
full pdf 2008
2) intestinalbarriertest.com/pdf/MaesGutBrainDepression.pdf
Neuroendocrinology Letters Volume 29 No. 1 2008
The gut-brain barrier in major depression: Intestinal mucosal dysfunction with an increased translocation of LPS from gram negative enterobacteria (leaky gut) plays a role in the inflammatory pathophysiology of depression
Michael Maes 1, Marta Kubera 2 and Jean-Claude Leunis 3 MCare4U Outpatient Clinics, Belgium; Department of Experimental Neuroendocrinology, Institute of Pharmacology, Polish Academy of Sciences, Krakow, Poland; Laboratory Ategis, Waver, Belgium. Correspondence to: Prof. Dr. M.Maes, M.D., Ph.D. Director: M-Care4U Outpatient Clinics, Olmenlaan 9, 2610 Antwerp, Belgium.
The findings of the present study show that MDD is accompanied by increased serum levels of IgM and IgA directed against LPS of gram-negative enterobacteria and that the IgM-IgA values are related to symptoms reminiscent of MDD and CFS, e.g. fatigue, autonomic and gastro-intestinal symptoms, and a subjective feeling of infection.
3) integrativehealthconnection.com/wp-content/uploads/2011/11/Leaky-gut-in-CFS-treatment-of-leaky-gut.pdf
Neuroendocrinology Letters Volume 29 No. 6 2008
Normalization of leaky gut in chronic fatigue syndrome (CFS) is accompanied by a clinical improvement: effects of age, duration of illness and the translocation of LPS from gram-negative bacteria Michael Maes 1,2, Jean-Claude Leunis 2 MCare4U Outpatient Clinics, Belgium
—————-
2008
4) www.ncbi.nlm.nih.gov/pubmed/18283240
Neuro Endocrinol Lett. 2008 Feb;29(1):117-24.
The gut-brain barrier in major depression: intestinal mucosal dysfunction with an increased translocation of LPS from gram negative enterobacteria (leaky gut) plays a role in the inflammatory pathophysiology of depression.
Maes M, Kubera M, Leunis JC. Source M-Care4U Outpatient Clinics, Antwerp, Belgium.
Abstract There is now evidence that major depression (MDD) is accompanied by an activation of the inflammatory response system (IRS) and that pro-inflammatory cytokines and lipopolysacharide (LPS) may induce depressive symptoms. The aim of the present study was to examine whether an increased gastrointestinal permeability with an increased translocation of LPS from gram negative bacteria may play a role in the pathophysiology of MDD. Toward this end, the present study examines the serum concentrations of IgM and IgA against LPS of the gram-negative enterobacteria, Hafnia Alvei, Pseudomonas Aeruginosa, Morganella Morganii, Pseudomonas Putida, Citrobacter Koseri, and Klebsielle Pneumoniae in MDD patients and normal controls. We found that the prevalences and median values for serum IgM and IgA against LPS of enterobacteria are significantly greater in patients with MDD than in normal volunteers. These differences are significant to the extent that a significant diagnostic performance is obtained, i.e. the area under the ROC curve is 90.1%. The symptom profiles of increased IgM and IgA levels are fatigue, autonomic and gastro-intestinal symptoms and a subjective feeling of infection. The results show that intestinal mucosal dysfunction characterized by an increased translocation of gram-negative bacteria (leaky gut) plays a role in the inflammatory pathophysiology of depression. It is suggested that the increased LPS translocation may mount an immune response and thus IRS activation in some patients with MDD and may induce specific “sickness behaviour” symptoms. It is suggested that patients with MDD should be checked for leaky gut by means of the IgM and IgA panel used in the present study and accordingly should be treated for leaky gut.
2012 chronic depression
5) www.ncbi.nlm.nih.gov/pubmed/22410503
J Affect Disord. 2012 Dec 1;141(1):55-62.
Increased IgA and IgM responses against gut commensals in chronic depression: further evidence for increased bacterial translocation or leaky gut.
Maes M, Kubera M, Leunis JC, Berk M. Source Maes Clinics @ Tria, Bangkok, Thailand.
Recently, we discovered that depression is accompanied by increased IgM and IgA responses directed against gram negative gut commensals. The aim of this study was to replicate these findings in a larger study group of depressed patients and to examine the associations between the IgA and IgM responses to gut commensals and staging of depression as well as the fatigue and somatic (F&S) symptoms of depression.
METHODS: We measured serum concentrations of IgM and IgA against the LPS of gram-negative enterobacteria, i.e. Hafnia alvei, Pseudomonas aeruginosa, Morganella morganii, Pseudomonas putida, Citrobacter koseri, and Klebsiella pneumoniae in 112 depressed patients and 28 normal controls. The severity of F&S symptoms was measured using the Fibromyalgia and Chronic Fatigue Syndrome Rating Scale.
RESULTS: The prevalences and median values of serum IgM and IgA against LPS of these commensals were significantly higher in depressed patients than in controls. The IgM levels directed against the LPS of these commensal bacteria were significantly higher in patients with chronic depression than in those without. The immune responses directed against LPS were not associated with melancholia or recurrent depression. There was a significant correlation between the IgA response directed against LPS and gastro-intestinal symptoms.
DISCUSSION: The results indicate that increased bacterial translocation with immune responses to the LPS of commensal bacteria may play a role in the pathophysiology of depression, particularly chronic depression.
Bacterial translocation may a) occur secondary to systemic inflammation in depression and intensify and perpetuate the primary inflammatory response once the commensals are translocated; or b) be a primary trigger factor associated with the onset of depression in some vulnerable individuals. The findings suggest that “translocated” gut commensal bacteria activate immune cells to elicit IgA and IgM responses and that this phenomenon may play a role in the pathophysiology of (chronic) depression by causing progressive amplifications of immune pathways.
2012 Chronic Fatigue Syndrome
6) www.ncbi.nlm.nih.gov/pubmed/21967891
J Affect Disord. 2012 Feb;136(3):909-17. Epub 2011 Oct 2.
Increased IgA responses to the LPS of commensal bacteria is associated with inflammation and activation of cell-mediated immunity in chronic fatigue syndrome.
Maes M, Twisk FN, Kubera M, Ringel K, Leunis JC, Geffard M. Source Maes Clinics @ TRIA, Bangkok, Thailand.
Abstract BACKGROUND: Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is accompanied by a) systemic IgA/IgM responses against the lipopolysaccharides (LPS) of commensal bacteria; b) inflammation, e.g. increased plasma interleukin-(IL)1 and tumor necrosis factor (TNF)a; and c) activation of cell-mediated immunity (CMI), as demonstrated by increased neopterin.
METHODS: To study the relationships between the IgA/IgM responses to the LPS of microbiota, inflammation, CMI and the symptoms of ME/CFS we measured the IgA/IgM responses to the LPS of 6 different enterobacteria, serum IL-1, TNFa, neopterin, and elastase in 128 patients with ME/CFS and chronic fatigue (CF). Severity of symptoms was assessed by the Fibromyalgia and Chronic Fatigue Syndrome (FF) Rating Scale.
RESULTS: Serum IL-1, TNFa, neopterin and elastase are significantly higher in patients with ME/CFS than in CF patients. There are significant and positive associations between the IgA responses to LPS and serum IL-1, TNFa, neopterin and elastase. Patients with an abnormally high IgA response show increased serum IL-1, TNFa and neopterin levels, and higher ratings on irritable bowel syndrome (IBS) than subjects with a normal IgA response. Serum IL-1, TNFa and neopterin are significantly related to fatigue, a flu-like malaise, autonomic symptoms, neurocognitive disorders, sadness and irritability. CONCLUSIONS: The findings show that increased IgA responses to commensal bacteria in ME/CFS are associated with inflammation and CMI activation, which are associated with symptom severity. It is concluded that increased translocation of commensal bacteria may be responsible for the disease activity in some ME/CFS patients.
2012 Emory Atlanta Dr Haroon
inflammation and depression
7) www.ncbi.nlm.nih.gov/pubmed/21918508 www.jain-resources.info/uploads/3/3/5/8/3358541/haroon_-_deplin_ds.pdf
Neuropsychopharmacology. 2012 Jan;37(1):137-62.
Psychoneuroimmunology meets neuropsychopharmacology: translational implications of the impact of inflammation on behavior.
Haroon E, Raison CL, Miller AH. Source Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, Atlanta, GA 30322, USA.
Abstract The potential contribution of chronic inflammation to the development of neuropsychiatric disorders such as major depression has received increasing attention. Elevated biomarkers of inflammation, including inflammatory cytokines and acute-phase proteins, have been found in depressed patients, and administration of inflammatory stimuli has been associated with the development of depressive symptoms. Data also have demonstrated that inflammatory cytokines can interact with multiple pathways known to be involved in the development of depression, including monoamine metabolism, neuroendocrine function, synaptic plasticity, and neurocircuits relevant to mood regulation. Further understanding of mechanisms by which cytokines alter behavior have revealed a host of pharmacologic targets that may be unique to the impact of inflammation on behavior and may be especially relevant to the treatment and prevention of depression in patients with evidence of increased inflammation. Such targets include the inflammatory signaling pathways cyclooxygenase, p38 mitogen-activated protein kinase, and nuclear factor-κB, as well as the metabolic enzyme, indoleamine-2,3-dioxygenase, which breaks down tryptophan into kynurenine. Other targets include the cytokines themselves in addition to chemokines, which attract inflammatory cells from the periphery to the brain. Psychosocial stress, diet, obesity, a leaky gut, and an imbalance between regulatory and pro-inflammatory T cells also contribute to inflammation and may serve as a focus for preventative strategies relevant to both the development of depression and its recurrence. Taken together, identification of mechanisms by which cytokines influence behavior may reveal a panoply of personalized treatment options that target the unique contributions of the immune system to depression.
8) www.ncbi.nlm.nih.gov/pmc/articles/PMC3038963/ www.biomedcentral.com/content/pdf/1757-4749-3-1.pdf
Gut Pathog. 2011; 3: 1.
Acne vulgaris, probiotics and the gut-brain-skin axis – back to the future?
Whitney P Bowe Alan C Logan
Department of Dermatology, State University of New York Downstate Medical Center, Brooklyn, New York, 11203, USA 2Integrative Care Centre of Toronto, 3600 Ellesmere Road, Unit 4, Toronto, ON M1C 4Y8, Canada
1999 Michael Maes
9) link.springer.com/chapter/10.1007%2F978-0-585-37970-8_2?LI=true
Cytokines, Stress, and Depression Advances in Experimental Medicine and Biology Volume 461, 1999, pp 25-46
Major Depression and Activation of The Inflammatory Response System Michael Maes M.D., Ph.D. Contemporary models of major depression emphasize the role of hypothalamic-pituitary-adrenal (HPA)-axis hyperactivity and of dysfunctions in the turnover of serotonin (5-HT) or catecholamines in the etiopathogenesis of major depression. Contemporary models of major depression do not incorporate the effects of the inflammatory response system (IRS), even though the IRS powerfully influences HPA-axis activity, 5-HT and catecholaminergic turnover and even though activation of the IRS may induce depression-like behavior in animals and humans. There is now evidence that major depression is accompanied by a moderate activation of the IRS (reviews: Maes, 1993; 1995; 1997; Maes, Smith, & Scharpe, 1995c; Holden, Pakula, & Mooney, 1997; Maes & Smith, 1997; Connor & Leonard, 1998; Maier & Watkins, 1998). In this paper we propose a concise IRS model of major depression.
—————————
10) pluto.huji.ac.il/~msrazy/PDF/MaesMetabBrainDis09.pdf
Metab Brain Dis. 2009 Mar;24(1):27-53. doi: 10.1007/s11011-008-9118-1. Epub 2008 Dec 16. The inflammatory & neurodegenerative (I&ND) hypothesis of depression: leads for future research and new drug developments in depression.
Maes M, Yirmyia R, Noraberg J, Brene S, Hibbeln J, Perini G, Kubera M, Bob P, Lerer B, Maj M. Source Clinical Research Center for Mental Health, Olmenlaan 9, Antwerp Wilrijk 2610, Belgium. neutrim@telenet.be
Abstract Despite extensive research, the current theories on serotonergic dysfunctions and cortisol hypersecretion do not provide sufficient explanations for the nature of depression. Rational treatments aimed at causal factors of depression are not available yet.
2011
11) www.ncbi.nlm.nih.gov/pubmed/20599581
Prog Neuropsychopharmacol Biol Psychiatry. 2011 Apr 29;35(3):664-75. doi: 10.1016/j.pnpbp.2010.06.014. Epub 2010 Jun 20.
Depression is an inflammatory disease, but cell-mediated immune activation is the key component of depression. Maes M.
The first findings that depression is characterized by cell-mediated immune activation and inflammation were published between 1990-1993 (Maes et al.). Recently, it was reported that–based on meta-analysis results–depression is an inflammatory disorder because the plasma levels of two cytokines are increased, i.e. interleukin-(IL)-6 and tumor necrosis factor-α (TNFα). The same meta-analysis found that plasma IL-2 and interferon-(IFN)γ levels are not altered in depression, suggesting that there is no T cell activation in that illness. The present paper reviews the body of evidence that depression is accompanied by cell-mediated immune activation. The findings include: increased serum levels of the soluble IL-2 receptor (sIL-2R) and the sCD8 molecule; increased numbers and percentages of T cells bearing T cell activation markers, such as CD2+CD25+, CD3+CD25+, and HLA-DR+; increased stimulated production of IFNγ; higher neopterin and sTNFR-1 or sTNFR-2 levels; induction of indoleamine 2,3-dioxygenase (IDO) with lowered levels of plasma tryptophan and increased levels of tryptophan catabolites along the IDO pathway (TRYCATs); and glucocorticoid resistance in immune cells. Interferon-α (IFNα)-based immunotherapy shows that baseline and IFNα-induced activation of T cells, IDO activity and TRYCAT formation are related to the development of IFNα-induced depressive symptoms. Animal models of depression show that a cell-mediated immune response is related to the development of depression-like behavior. Antidepressants and mood stabilizers suppress different aspects of cell-mediated immunity and rather specifically target IFNγ production. This review shows that inflammation and cell-mediated immune activation are key factors in depression.
12) www.ncbi.nlm.nih.gov/pubmed/21930301
J Affect Disord. 2011 Dec;135(1-3):414-8.
IgM-mediated autoimmune responses directed against multiple neoepitopes in depression: new pathways that underpin the inflammatory and neuroprogressive pathophysiology. Maes M, Mihaylova I, Kubera M, Leunis JC, Geffard M. Source Maes Clinics @ TRIA, Bangkok, Thailand. dr.michaelmaes@hotmail.com
Abstract BACKGROUND: There is evidence that depression is accompanied by oxidative and nitrosative stress (O&NS), as indicated by increased free radical levels, lipid peroxidation, and lowered antioxidant levels. The aims of the present study are to examine whether depression is accompanied by autoimmune responses directed against a) neoepitopes that are formed following O&NS damage; and b) the major anchorage molecules, i.e. palmitic and myristic acids and S- farnesyl-L-cysteine.
METHODS: We examined serum IgM antibodies to the conjugated fatty acids, palmitic and myristic acids; acetylcholine; S-farnesyl-L-cysteine; and NO-modified adducts in 26 depressed patients and 17 normal controls. Severity of depression was measured with the Hamilton Depression Rating Scale and severity of fatigue and somatic (F&S) symptoms with the Fibromyalgia and Chronic Fatigue Syndrome (FF) Rating Scale.
RESULTS: The prevalences and mean values for the serum IgM levels directed against conjugated palmitic and myristic acids, acetylcholine, S-farnesyl-L-cysteine; and the conjugated NO adducts, NO-tyrosine, NO-phenylalanine, NO-aspartate, NO-histidine, and NO-creatine were significantly higher in depressed patients than in normal controls. The autoimmune responses were significantly related to FF symptoms, such as fatigue and a flu-like malaise, whereas the indicants of nitrosative stress were related to gastro-intestinal and autonomic symptoms.
DISCUSSION: Depression is characterized by IgM-related autoimmune responses directed against a) neoepitopes that are normally not detected by the immune system but that due to damage by O&NS have become immunogenic; and b) anchorage epitopes, i.e. palmitic and myristic acids, and S-farnesyl-L-cysteine. These autoimmune responses play a role in the inflammatory and O&NS pathophysiology of depression and may mediate the cellular dysfunctions that contribute to neuroprogression, e.g. aberrations in signal transduction, cellular differentiation and apoptosis.
13) www.ncbi.nlm.nih.gov/pubmed/21945535
Prog Neuropsychopharmacol Biol Psychiatry. 2012 Jan 10;36(1):169-75. doi: 10.1016/j.pnpbp.2011.09.006. Epub 2011 Sep 16.
Activation of cell-mediated immunity in depression: association with inflammation, melancholia, clinical staging and the fatigue and somatic symptom cluster of depression. Maes M, Mihaylova I, Kubera M, Ringel K. Source Maes Clinics @ TRIA, Bangkok, Thailand. dr.michaelmaes@hotmail.com
Abstract BACKGROUND: Depression is characterized by activation of cell-mediated immunity (CMI), including increased neopterin levels, and increased pro-inflammatory cytokines (PICs), such as interleukin-1 (IL-1) and tumor necrosis factor-α (TNFα). These PICs may induce depressive, melancholic and chronic fatigue (CF) symptoms.
METHODS: We examined serum neopterin and plasma PIC levels in depressive subgroups in relation to the depressive subtypes and the melancholic and CF symptoms of depression. Participants were 85 patients with depression and in 26 normal controls. Severity of depression was assessed with the Hamilton Depression Rating Scale (HDRS) and severity of CF with the Fibromyalgia and Chronic Fatigue Syndrome (FF) Rating Scale.
RESULTS: Serum neopterin was significantly higher in depressed patients and in particular in those with melancholia. There were positive correlations between serum neopterin, the plasma PICs and the number of previous depressive episodes. Neopterin and TNFα were associated with melancholia, while both PICs were associated with CF. Melancholia-group membership was predicted by the HDRS and neopterin, and CF group membership by age, the FF score and serum TNFα.
DISCUSSION: Depression and melancholia are accompanied by CMI activation, suggesting that neopterin plays a role in their pathophysiology, e.g. through activation of oxidative and nitrosative stress and apoptosis pathways. The intertwined CMI and inflammatory responses are potentially associated with the onset of depression and with the melancholic and CF symptoms of depression. Exposure to previous depressive episodes may magnify the size of CMI and PIC responses, possibly increasing the likelihood of new depressive episodes. CMI activation and inflammation may contribute to the staging or recurrence of depression.
14) www.ncbi.nlm.nih.gov/pubmed/20471444
Prog Neuropsychopharmacol Biol Psychiatry. 2011 Apr 29;35(3):676-92. doi: 10.1016/j.pnpbp.2010.05.004. Epub 2010 May 12.
A review on the oxidative and nitrosative stress (O&NS) pathways in major depression and their possible contribution to the (neuro)degenerative processes in that illness.
Maes M, Galecki P, Chang YS, Berk M. Source Maes@TRIA Clinics, Bangkok, Thailand. dr.michaelmaes@hotmail.com
Abstract This paper reviews the body of evidence that major depression is accompanied by a decreased antioxidant status and by induction of oxidative and nitrosative (IO&NS) pathways. Major depression is characterized by significantly lower plasma concentrations of a number of key antioxidants, such as vitamin E, zinc and coenzyme Q10, and a lowered total antioxidant status. Lowered antioxidant enzyme activity, e.g. glutathione peroxidase (GPX), is another hallmark of depression. The abovementioned lowered antioxidant capacity may impair protection against reactive oxygen species (ROS), causing damage to fatty acids, proteins and DNA by oxidative and nitrosative stress (O&NS). Increased ROS in depression is demonstrated by increased levels of plasma peroxides and xanthine oxidase. Damage caused by O&NS is shown by increased levels of malondialdehyde (MDA), a by-product of polyunsaturated fatty acid peroxidation and arachidonic acid; and increased 8-hydroxy-2-deoxyguanosine, indicating oxidative DNA damage. There is also evidence in major depression, that O&NS may have changed inactive autoepitopes to neoantigens, which have acquired immunogenicity and serve as triggers to bypass immunological tolerance, causing (auto) immune responses. Thus, depression is accompanied by increased levels of plasma IgG antibodies against oxidized LDL; and increased IgM-mediated immune responses against membrane fatty acids, like phosphatidyl inositol (Pi); oleic, palmitic, and myristic acid; and NO modified amino-acids, e.g. NO-tyrosine, NO-tryptophan and NO-arginine; and NO-albumin. There is a significant association between depression and polymorphisms in O&NS genes, like manganese superoxide dismutase, catalase, and myeloperoxidase. Animal models of depression very consistently show lowered antioxidant defences and activated O&NS pathways in the peripheral blood and the brain. In animal models of depression, antidepressants consistently increase lowered antioxidant levels and normalize the damage caused by O&NS processes. Antioxidants, such as N-acetyl-cysteine, compounds that mimic GPX activity, and zinc exhibit antidepressive effects. This paper reviews the pathways by which lowered antioxidants and O&NS may contribute to depression, and the (neuro)degenerative processes that accompany that illness. It is concluded that aberrations in O&NS pathways are–together with the inflammatory processes–key components of depression. All in all, the results suggest that depression belongs to the spectrum of (neuro)degenerative disorders.
15) www.ncbi.nlm.nih.gov/pubmed/20035260
Neuro Endocrinol Lett. 2009;30(6):715-22.
Increased 8-hydroxy-deoxyguanosine, a marker of oxidative damage to DNA, in major depression and myalgic encephalomyelitis / chronic fatigue syndrome.
Maes M, Mihaylova I, Kubera M, Uytterhoeven M, Vrydags N, Bosmans E. Source Maes Clinics, Wilrijk – Antwerp, Belgium. crc.mh@telenet.be
Abstract BACKGROUND: There is now evidence that major depression and myalgic encephalomyelitis / chronic fatigue syndrome (ME/CFS) are accompanied by partially overlapping pathophysiological mechanisms, i.e. activation of various inflammatory and oxidative & nitrosative (IO&NS) pathways. OBJECTIVE: The aim of the present study was to examine the urinary excretion of 8-hydroxy-deoxyguanosine (![]() hdG), a marker of oxidative damage to DNA, in depression; ME/CFS; and depression and ME/CFS. METHODS: Toward this end, morning urine was sampled for the assays of
hdG), a marker of oxidative damage to DNA, in depression; ME/CFS; and depression and ME/CFS. METHODS: Toward this end, morning urine was sampled for the assays of ![]() HdG and creatinine, in 44 patients with ME/CFS; 25 with major depression; 23 with depression and ME/CFS; and 17 normal controls. Severity of fatigue and somatic symptoms was measured by means of the Fibromyalgia and CFS Rating (FF) scale. RESULTS: We found that 49.0% of the variance in the urinary excretion of
HdG and creatinine, in 44 patients with ME/CFS; 25 with major depression; 23 with depression and ME/CFS; and 17 normal controls. Severity of fatigue and somatic symptoms was measured by means of the Fibromyalgia and CFS Rating (FF) scale. RESULTS: We found that 49.0% of the variance in the urinary excretion of ![]() HdG was predicted by the regression on creatinine. Consequently, the urinary
HdG was predicted by the regression on creatinine. Consequently, the urinary ![]() HdG excretion should be expressed as the residualized
HdG excretion should be expressed as the residualized ![]() HdG values after partialling out the effects of creatinine and not by computing the
HdG values after partialling out the effects of creatinine and not by computing the ![]() HdG / creatinine ratio. We found that the residualized urinary excretion of
HdG / creatinine ratio. We found that the residualized urinary excretion of ![]() HdG (adjusted for creatinine) was significantly higher in patients with depression and ME/CFS than in normal controls and all other patients. In the patient group, there were significant correlations between the urinary
HdG (adjusted for creatinine) was significantly higher in patients with depression and ME/CFS than in normal controls and all other patients. In the patient group, there were significant correlations between the urinary ![]() HdG and the total score on the FF scale and sadness and flu-like malaise. CONCLUSIONS: The findings show increased oxidatively generated DNA damage in patients with major depression and ME/CFS and, therefore, further extent the role played by IO&NS pathways in the pathophysiology of both disorders. Since oxidatively damage to DNA is a risk factor for atherosclerosis and neurodegeneration, our results also explain previous findings on increased cardiovascular morbidity in depression and ME/CFS, and neurodegenerative processes in depression. ———————-
HdG and the total score on the FF scale and sadness and flu-like malaise. CONCLUSIONS: The findings show increased oxidatively generated DNA damage in patients with major depression and ME/CFS and, therefore, further extent the role played by IO&NS pathways in the pathophysiology of both disorders. Since oxidatively damage to DNA is a risk factor for atherosclerosis and neurodegeneration, our results also explain previous findings on increased cardiovascular morbidity in depression and ME/CFS, and neurodegenerative processes in depression. ———————-
16) www.triaintegrativewellness.com/leaky-gut-a-potentially-dangerous-but-treatable-condition/
article by Michael Maes, M.D., Ph.D. Leaky gut: a potentially dangerous but treatable condition When you suffer from an impaired transit, diarrhea or constipation, bloating, and intestinal cramps, it may be that you suffer from leaky gut.
———
17) dralexrinehart.com/nutrition-benefits/does-leaky-gut-exist/
Does Leaky Gut Exist? Written on April 4, 2012 by Dr. Alexander Rinehart, MS, DC, CCN in Nutrition Benefits When a gastroenterologist or other health professional claims that “leaky gut does not exist”, I cringe. I believe that they are really stating that, in their opinion, leaky gut has no scientific basis. I personally feel that such bold claims are a discriminatory technique used against alternative providers such as Naturopathic doctors, Chiropractors and Nutritionists who are increasingly seeing clients for problems once restricted to medical care.
18) syontix.com/why-do-i-feel-so-blue-the-role-of-endotoxemia-and-leaky-gut-in-the-cause-of-major-depression/ Why Do I Feel So Blue? The Role of Endotoxemia and Leaky Gut in the Cause of Major Depression Published October 14, 2012 | By Ray Medina
19) leakygutsyndrometreatment.net/healing-leaky-gut-syndrome/
Healing Leaky Gut Syndrome
Multiple SClerosis and Leaky Gut
20) www.msrc.co.uk/index.cfm/fuseaction/show/pageid/737
Leaky Gut and MS Leaky Gut
There are many parties that are convinced that increased intestinal permeability or a leaky gut may be connected to a good many people with Multiple Sclerosis. The MS Diet Research Group connected to the Best Bet Diet Group are making progress getting academics and doctors interested in researching this field as to date only very limited research has been carried out. Having said that the results of this research have indicated a plausible connection. If is also people with MS themselves who are proving that measures taken to heal the gut can often result in improvement in their MS symptoms.
21) sanjosefuncmed.com/intestinal-permeability-leaky-gut/
What is Intestinal Permeability or “Leaky Gut”? What is intestinal permeability or “leaky gut”? Why haven’t I heard of this? Intestinal permeability causes systemic inflammation. Intestinal permeability as a precondition for the development of autoimmune disease.
22) www.ncbi.nlm.nih.gov/pubmed/21278760 www.iem.cas.cz/miranda2/export/sitesavcr/data.avcr.cz/lifesci/uem/research/publications/pharmacology/files/tlaskalova-hogenova-2011.pdf Cell Mol Immunol. 2011 Mar;8(2):110-20. doi: 10.1038/cmi.2010.67. Epub 2011 Jan 31.
The role of gut microbiota (commensal bacteria) and the mucosal barrier in the pathogenesis of inflammatory and autoimmune diseases and cancer: contribution of germ-free and gnotobiotic animal models of human diseases.
Tlaskalová-Hogenová H, Stěpánková R, Kozáková H, Hudcovic T, Vannucci L, Tučková L, Rossmann P, Hrnčíř T, Kverka M, Zákostelská Z, Klimešová K, Přibylová J, Bártová J, Sanchez D, Fundová P, Borovská D, Srůtková D, Zídek Z, Schwarzer M, Drastich P, Funda DP. Source Institute of Microbiology, Academy of Sciences of the Czech Republic, v.v.i., Prague, Czech Republic. tlaskalo@biomed.cas.cz Abstract
Metagenomic approaches are currently being used to decipher the genome of the microbiota (microbiome), and, in parallel, functional studies are being performed to analyze the effects of the microbiota on the host. Gnotobiological methods are an indispensable tool for studying the consequences of bacterial colonization. Animals used as models of human diseases can be maintained in sterile conditions (isolators used for germ-free rearing) and specifically colonized with defined microbes (including non-cultivable commensal bacteria). The effects of the germ-free state or the effects of colonization on disease initiation and maintenance can be observed in these models. Using this approach we demonstrated direct involvement of components of the microbiota in chronic intestinal inflammation and development of colonic neoplasia (i.e., using models of human inflammatory bowel disease and colorectal carcinoma). In contrast, a protective effect of microbiota colonization was demonstrated for the development of autoimmune diabetes in non-obese diabetic (NOD) mice. Interestingly, the development of atherosclerosis in germ-free apolipoprotein E (ApoE)-deficient mice fed by a standard low-cholesterol diet is accelerated compared with conventionally reared animals. Mucosal induction of tolerance to allergen Bet v1 was not influenced by the presence or absence of microbiota. Identification of components of the microbiota and elucidation of the molecular mechanisms of their action in inducing pathological changes or exerting beneficial, disease-protective activities could aid in our ability to influence the composition of the microbiota and to find bacterial strains and components (e.g., probiotics and prebiotics) whose administration may aid in disease prevention and treatment.
—————–
PArkinson’s Diease and Leaky Gut
23) www.ncbi.nlm.nih.gov/pmc/articles/PMC3228722/ www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0028032
PLoS One. 2011; 6(12): e28032. Published online 2011 December 1. doi: 10.1371/journal.pone.0028032 PMCID: PMC3228722 Increased Intestinal Permeability Correlates with Sigmoid Mucosa alpha-Synuclein Staining and Endotoxin Exposure Markers in Early Parkinson’s Disease Christopher B. Forsyth,1,* Kathleen M. Shannon,2 Jeffrey H. Kordower,3 Robin M. Voigt,1 Maliha Shaikh,1 Jean A. Jaglin,2 Jacob D. Estes,4 Hemraj B. Dodiya,3 and Ali Keshavarzian1 1Department of Internal Medicine, Section of Gastroenterology, Rush University Medical Center, Chicago, Illinois, United States of America 2Department of Neurological Sciences, Rush University Medical Center, Chicago, Illinois, United States of America 3Center for Brain Repair, Rush Medical College, Chicago, Illinois, United States of America 4AIDS and Cancer Virus Program, SAIC-Frederick, Inc., National Cancer Institute-Frederick, Frederick, Maryland, United States of America University Hospital La Paz, Spain
Parkinson’s disease (PD) is the second most common neurodegenerative disorder of aging. The pathological hallmark of PD is neuronal inclusions termed Lewy bodies whose main component is alpha-synuclein protein. The finding of these Lewy bodies in the intestinal enteric nerves led to the hypothesis that the intestine might be an early site of PD disease in response to an environmental toxin or pathogen. One potential mechanism for environmental toxin(s) and proinflammatory luminal products to gain access to mucosal neuronal tissue and promote oxidative stress is compromised intestinal barrier integrity. However, the role of intestinal permeability in PD has never been tested. We hypothesized that PD subjects might exhibit increased intestinal permeability to proinflammatory bacterial products in the intestine. To test our hypothesis we evaluated intestinal permeability in subjects newly diagnosed with PD and compared their values to healthy subjects. In addition, we obtained intestinal biopsies from both groups and used immunohistochemistry to assess bacterial translocation, nitrotyrosine (oxidative stress), and alpha-synuclein. We also evaluated serum markers of endotoxin exposure including LPS binding protein (LBP). Our data show that our PD subjects exhibit significantly greater intestinal permeability (gut leakiness) than controls.
In addition, this intestinal hyperpermeability significantly correlated with increased intestinal mucosa staining for E. coli bacteria, nitrotyrosine, and alpha-synuclein as well as serum LBP levels in PD subjects.
These data represent not only the first demonstration of abnormal intestinal permeability in PD subjects but also the first correlation of increased intestinal permeability in PD with intestinal alpha–synuclein (the hallmark of PD), as well as staining for gram negative bacteria and tissue oxidative stress. Our study may thus shed new light on PD pathogenesis as well as provide a new method for earlier diagnosis of PD and suggests potential therapeutic targets in PD subjects.
———————-
Cyrex LAbs- IgM and IgG antibodies to LPS, gluten panels, autoimmune panels
www.cyrexlabs.com/Portals/0/Docs/ClinicalApplications/ClinicalAppArray2.pdf
Clinical Application Guide
www.cyrexlabs.com/Portals/0/Docs/ClinicalApplications/ClinicalAppArray5.pdf AUtoimmune Screen
http://www.biobotanicalresearch.com/
BioBotanical Research
Biocidin/Olivex
Jeffrey Dach MD
7450 Griffin Road, Suite 190
Davie, Fl 33314
954-792-4663
www.jeffreydach.com
www.drdach.com
www.naturalmedicine101.com
www.bioidenticalhormones101.com
www.truemedmd.com
Click Here for: Dr Dach’s Online Store for Pure Encapsulations Supplements
Click Here for: Dr Dach’s Online Store for Nature’s Sunshine Supplements
Web Site and Discussion Board Links:
jdach1.typepad.com/blog/
disc.yourwebapps.com/Indices/244124.html
disc.yourwebapps.com/Indices/244066.html
disc.yourwebapps.com/Indices/244067.html
disc.yourwebapps.com/Indices/244161.html
disc.yourwebapps.com/Indices/244163.html
Disclaimer click here: www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship. Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Link to this article:http://wp.me/P3gFbV-1u
Copyright (c) 2013 Jeffrey Dach MD All Rights Reserved. This article may be reproduced on the internet without permission, provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.
Leave a Comment
You must be logged in to post a comment.