 Testosterone Erythrocytosis Thrombophilia and Heart Attack by Jeffrey Dach MD
Testosterone Erythrocytosis Thrombophilia and Heart Attack by Jeffrey Dach MD
My previous article part one and part two discussed recent studies showing increased heart attack rates in men starting testosterone. Recently there have been two more reports by Dr. Finkle and Dr Vigen confirming, yes, this is a real finding (6,7). Rather than point out methodological flaws in Dr. Vigen’s study, as in the letter by Dr Abraham Morgentaler to JAMA, I think the findings should be taken at face value. (8) If so, then what is the explanation ?
Erythocytosis and Myocardial Infarction
 Practitioners who routinely prescribe testosterone to men will notice a common lab abnormality. Elevations of hemoglobin, hematocrit, iron and ferritin may be mild moderate or severe. This is well known.
Practitioners who routinely prescribe testosterone to men will notice a common lab abnormality. Elevations of hemoglobin, hematocrit, iron and ferritin may be mild moderate or severe. This is well known.
Testosterone Elevates the Blood Count
Testosterone causes erythrocytosis and will elevate the blood count causing thickening of the blood and sluggish blood flow.(9-11) The mechanism has been elucidated as a stimulation of erythropoetin, which in turn, stimulates the bone marrow to produce more blood cells. In addition, testosterone therapy suppresses Hepcidin. This will increase Iron Transport, causing more iron to be made available for red cell production, with elevation of serum iron and ferritin.(9-10) Erythrocytosis, in itself, is a risk factor for coronary artery disease, treatable with blood donation at the blood bank. (1-5)(9-11)
None of the testosterone studies actually reported the incidence or treatment of erythrocytosis in their population. Monitoring blood count and regular blood donations to reduce iron stores is an important part of the treatment protocol which was omitted in these studies.
Thrombophilia
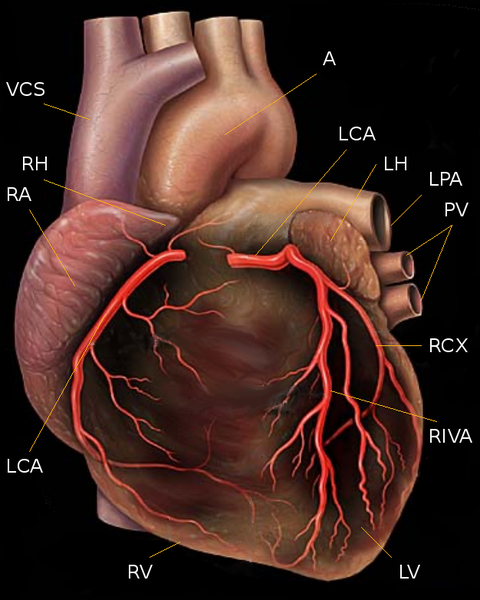
Secondly, some men have had hereditary thrombophilia which increases the tendency of their blood to form thrombus, or clots. Testosterone induced erythrocytosis may unmask men in this group who may go on to form thrombus in areas of critical vascular stenosis, as in the men with underlying coronary artery disease.(6,7) (12-18)
Genetic abnormalities may include Factor V Leiden, MTHFR, polymorphism in the PAI-1 gene locus 4G/5G, and polymorphism in the Angiotensin Converting Enzyme gene (ACE), increased lipoprotein (a), etc. all of which may be associated with increased risk for heart disease. (12-18)
Health Benefits of Testosterone
Many long term studies have shown conclusively that low testosterone levels are associated with increase risk of cardiovascular mortality, and testosterone therapy reduces mortality in this group, as discussed in my previous article. The benefits of testosterone therapy were especially striking in the diabetic group.
In conclusion: An explanation, which has yet to be confirmed, is the hypothesis that starting testosterone therapy in men with underlying coronary artery disease may unmask those with hereditary thombophilia. These men are at greater risk of thrombosis associated with erythrocytosis, a well known adverse effect of testosterone therapy, easily treatable with regular donations at the blood bank.
Early MI in Young Male: Testing protocol
Testing protocols include the following: lipoprotein(a), homocysteine, antiphospholipid antibodies, plasminogen activator inhibitor-1, factor V Leiden mutation, prothrombin variant, and 5,10-methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism, etc.
Update 9/12/14: Connection between hereditary thrombophilia and DVT in men taking testosterone: Testosterone Therapy, Thrombophilia–Hypofibrinolysis, and Hospitalization for Deep Venous Thrombosis-Pulmonary Embolus: An Exploratory, Hypothesis-Generating Study Charles J. Glueck, MD
Articles with Related Content
Health Benefits of Regular Blood Donation
Testosterone and the Heart Part One
Testosterone and the Heart Part Two
Jeffrey Dach MD
7450 Griffin Road, Suite 190
Davie, Fl 33314
954-792-4663
www.jeffreydach.com
www.drdach.com
www.naturalmedicine101.com
www.bioidenticalhormones101.com
www.truemedmd.com
Links and References
1) http://www.ncbi.nlm.nih.gov/
Anabolic steroids, acute myocardial infarction and polycythemia: A case report and review of the literature
Stergiopoulos, Kathleen, et al. Vascular health and risk management 4.6 (2008): 1475.
2) http://www.ijge-online.com/
International Journal of Gerontology Volume 6, Issue 4 , Pages 290-291, December 2012
Erythrocytosis Secondary to Testosterone Therapy in a Male with Cryptorchidism: A Case Report☆☆☆
Summary Hypogonadism is association with aging (andropause) can now be recognized earlier and treated with testosterone, thus resulting in the relief of symptoms and better quality of life. However, any patients that are treated with testosterone must be closely monitored in order to avoid the development of sleep apnea, cardiovascular diseases, hepatic dysfunction, plasma lipid disorders, or erythrocytosis, all of which are potential side effects of treatment. Herein, we present a case of erythrocytosis secondary to testosterone treatment in a patient with cryptorchidism. Hemoglobin levels returned to normal soon after phlebotomy and discontinuation of testosterone therapy. Physicians should be aware of the side effects of testosterone replacement therapy and cautiously monitor patients in order to avoid these side effects and cumbersome and expensive laboratory tests.
3) http://www.ncbi.nlm.nih.gov/
Herz. 2006 Sep;31(6):566-73.
[Cardiovascular side effects of anabolic-androgenic steroids].
[Article in German]Kindermann W.
The intake of anabolic-androgenic steroids (AAS) leads to an increase in skeletal muscle mass and is prohibited as a doping measure in sport. AAS abuse is not limited to competitive athletes. It is also prevalent in subjects who do body building or resistance training for cosmetic reasons only. Out of the numerous and partly serious side effects, the cardiovascular ones are presented here. An increase in left ventricular muscle mass is well documented, and some researchers have even reported concentric hypertrophy. By contrast, resistance training without AAS intake does not lead to increased ventricular wall thickness. AAS do not affect the systolic function of the left ventricle, whereas diastolic function might be impaired. Different ultrastructural myocardial alterations have been documented in animal studies. In addition, AAS can induce arterial hypertension. Blood clotting and fibrinolysis are negatively affected, and several case studies of thrombi exist in young strength athletes. Changes in the concentration of blood lipoproteins, particularly a reduction in vessel-protective HDL cholesterol, can lead to early atherosclerosis. Many case reports exist about cardiac deaths in seemingly healthy subjects-most often body builders and other strength athletes. In fatal and nonfatal myocardial infarctions patent coronary arteries were proven frequently. Besides the prothrombotic effects of AAS, an impaired endothelial function and vasospasms are discussed hypothetically as pathomechanisms. Also, cardiomyopathies can occur due to AAS abuse. On the basis of the described possible cardiovascular side effects, it can be concluded that in cases of sudden cardiac deaths in young athletes, a misuse of AS should be excluded.
4) http://archinte.jamanetwork.
Myocardial Infarction as the Initial Manifestation of Polycythemia Vera
JOSEPH B. VACCA, M.D.; GEORGE E. THOMA Jr., M.D.
AMA Arch Intern Med. 1959;103(6):974-977.
5) http://www.ncbi.nlm.nih.gov/
J Intern Med. 1998 Jul;244(1):49-53.
Acute coronary disease in essential thrombocythemia and polycythemia vera.
Rossi C, Randi ML, Zerbinati P, Rinaldi V, Girolami A.
The aim of this study is to report our experience on myocardial infarction (MI) in patients with essential thrombocythemia (ET) and polycythemia vera (PV).
DESIGN:Patients with PV and ET consecutively diagnosed and followed in authors’ Department between 1 July 1986 and 30 June 1996.
SUBJECTS:Over the past 10 years we have followed 170 patients with ET and 149 with PV, diagnosed according to the Polycythemia Vera Study Group (PVSG) criteria. The patients were divided into 3 groups on the basis of the age at diagnosis (group A < 40, B 41-65, C > 65 years).
INTERVENTIONS:In all patients with PV phlebotomies and/or myelosuppressive therapy were used to keep haematocrit level lower than 45%. Hydroxyurea was given to patients with ET with a positive history for major vascular complications or with an extreme thrombocytosis. Aspirin therapy (ASA) (100 mg per day) was administered in patients with microvascular disturbances or previous thrombosis (in patients with PV also in the presence of atherosclerotic risk factors).
MAIN OUTCOME MEASURES:Frequency of MI in patients with ET and PV with and without ASA therapy.
RESULTS:9.4% of patients with ET and 11.4% of those with PV had MI. 17.6% of patients with PV were younger than 40 years at the moment of MI in contrast to 0% of those with ET. 75% of patients with ET and 70.6% of those with PV with MI had atherosclerotic risk factors such as smoking, hypertension, diabetes, dyslipidaemia. All patients with MI received ASA 100 mg daily after thrombosis and four of the ET group developed a transient ischaemic attack (TIA) afterwards. Four subjects with PV during the follow-up had TIAs and two peripheral arteriopathy in spite of ASA treatment.
CONCLUSIONS:MI is less common in patients with ET younger than 40 years than in older patients. Association of MI and cardiovascular risk factors is frequent in patients with ET and PV. A low dose of ASA could be able to reduce the number of coronary thrombosis without increasing bleeding complications in patients with elevated platelet count and common atherosclerotic risk factors. However, a larger population must be evaluated to confirm our hypothesis.
——————————
Finkle, William D., et al. “Increased Risk of Non-Fatal Myocardial Infarction Following Testosterone Therapy Prescription in Men.” PLoS ONE 9.1 (2014).
Published: January 29, 2014
7) http://www.ncbi.nlm.nih.gov/
JAMA. 2013 Nov 6;310(17):1829-36. doi: 10.1001/jama.2013.280386.
Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels.
Vigen R, O’Donnell CI, Barón AE, Grunwald GK, Maddox TM, Bradley SM, Barqawi A, Woning G, Wierman ME, Plomondon ME, Rumsfeld JS, Ho PM.
Rates of testosterone therapy are increasing and the effects of testosterone therapy on cardiovascular outcomes and mortality are unknown. A recent randomized clinical trial of testosterone therapy in men with a high prevalence of cardiovascular diseases was stopped prematurely due to adverse cardiovascular events raising concerns about testosterone therapy safety.
OBJECTIVES:To assess the association between testosterone therapy and all-cause mortality, myocardial infarction (MI), or stroke among male veterans and to determine whether this association is modified by underlying coronary artery disease.
DESIGN, SETTING, AND PATIENTS:A retrospective national cohort study of men with low testosterone levels (<300 ng/dL) who underwent coronary angiography in the Veterans Affairs (VA) system between 2005 and 2011.
MAIN OUTCOMES AND MEASURES:Primary outcome was a composite of all-cause mortality, MI, and ischemic stroke.
RESULTS:Of the 8709 men with a total testosterone level lower than 300 ng/dL, 1223 patients started testosterone therapy after a median of 531 days following coronary angiography. Of the 1710 outcome events, 748 men died, 443 had MIs, and 519 had strokes. Of 7486 patients not receiving testosterone therapy, 681 died, 420 had MIs, and 486 had strokes. Among 1223 patients receiving testosterone therapy, 67 died, 23 had MIs, and 33 had strokes. The absolute rate of events were 19.9% in the no testosterone therapy group vs 25.7% in the testosterone therapy group, with an absolute risk difference of 5.8% (95% CI, -1.4% to 13.1%) at 3 years after coronary angiography. In Cox proportional hazards models adjusting for the presence of coronary artery disease, testosterone therapy use as a time-varying covariate was associated with increased risk of adverse outcomes (hazard ratio, 1.29; 95% CI, 1.04 to 1.58). There was no significant difference in the effect size of testosterone therapy among those with and without coronary artery disease (test for interaction, P = .41).
CONCLUSIONS AND RELEVANCE:Among a cohort of men in the VA health care system who underwent coronary angiography and had a low serum testosterone level, the use of testosterone therapy was associated with increased risk of adverse outcomes. These findings may inform the discussion about the potential risks of testosterone therapy.
8) Morgenthaler Letter to JAMA
Morgentaler_Vigen_testosterone_VA_heart_JAMA-ltr-2
To anyone familiar with the testosterone field, the results reported by Vigen et al1 were surprising, alleging increased deaths and cardiovascular events in a group of VA men receiving testosterone following coronary angiography, contradicting a rich literature spanning 20+ years.2 Should testosterone therapy be considered unsafe based on this article? The short answer is no. This was not a straightforward two-group comparison in which events were higher in men who received testosterone. Rather, this was a complex retrospective study with a messy dataset, containing a fatal flaw that distorted the conclusion.
The authors wrote, “The absolute rate of events were 19.9% in the no testosterone therapy group vs 25.7% in the testosterone therapy group” at 3y following angiography. This is impossible since the raw rate of events in the T group was only 10.1% (123 events in 1223 men) , compared with 21.2% (1587 events in 7486 men) in the no-T group. The authors never acknowledge these data favoring the T-group, nor do they explain what drove results to an opposite conclusion. The Kaplan-Meier curves are similarly misleading, as the approximately 30% event rate for the T-group at the end of the study is a 3x multiple of the actual event rate. We assume the disparity is derived from calculated estimates based on statistical adjustment for >50 variables, thus magnifying potential errors.
Both groups began as a single population, with men joining the T-group as they began treatment, thus contributing to both event curves. An MI was attributed to the T group if a man filled his testosterone prescription the same day, but to the no-T group if he hadn’t yet filled it. Attempts to glean clarity from chaos using statistics is laudable, yet as anyone with a teenager knows, there is a large difference between what is expected and what actually occurs.
Basic information is not provided. Did time-zero begin for T-group at angiography or testosterone initiation? Raw event data for years 1-3? Mean time to events after testosterone? Person-years of exposure for both groups?
Our greatest concern is that 1132 men with MI or stroke who subsequently received testosterone were incorrectly excluded from the study. It was irrelevant what happened after their event. All these events occurred in the no-T group, increasing its number of events by 71%, thereby yielding an outcome consistent with two recent studies demonstrating a substantial reduction in mortality with testosterone therapy.3,4
Abraham Morgentaler, MD
Abdulmaged Traish, PhD
Ravi Kacker, MD
References
1. Vigen R, O’Donnell CI, Baron AE, et al. Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA 2013 ; 310:1829-36.
2. Traish AM, Miner MM, Morgentaler A, Zitzmann M. Testosterone deficiency. Am J Med 2011; 123:578-87.
3. Shores MM, Smith NL, Forsberg CW, Anawalt BD, Matsumoto AM. Testosterone treatment and mortality in men with low testosterone levels. J Clin Endocrin Metab 2012 ; 97:2050-8.
4. Muraleedharan V, Marsh H, Kapoor D, Channers KS, Jones TH. Testosterone deficiency is associated with increased risk of mortality and testosterone replacement improves survival in men with type 2 diabetes. Eur J Endocrin 2013; 169:725-33.
——————————
9) http://biomedgerontology.
Testosterone Induces Erythrocytosis via Increased Erythropoietin and Suppressed Hepcidin: Evidence for a New Erythropoietin/Hemoglobin Set Point
10) http://www.ncbi.nlm.nih.gov/
J Gerontol A Biol Sci Med Sci. 2013 Oct 24. [Epub ahead of print]
Testosterone Induces Erythrocytosis via Increased Erythropoietin and Suppressed Hepcidin: Evidence for a New Erythropoietin/Hemoglobin Set Point.
Bachman E, Travison TG, Basaria S, Davda MN, Guo W, Li M, Connor Westfall J, Bae H, Gordeuk V, Bhasin S.
The mechanisms by which testosterone increases hemoglobin and hematocrit remain unclear.
METHODS:We assessed the hormonal and hematologic responses to testosterone administration in a clinical trial in which older men with mobility limitation were randomized to either placebo or testosterone gel daily for 6 months.
RESULTS:The 7%-10% increase in hemoglobin and hematocrit, respectively, with testosterone administration was associated with significantly increased erythropoietin (EPO) levels and decreased ferritin and hepcidin levels at 1 and 3 months. At 6 months, EPO and hepcidin levels returned toward baseline in spite of continued testosterone administration, but EPO levels remained nonsuppressed even though elevated hemoglobin and hematocrit higher than at baseline, suggesting a new set point. Consistent with increased iron utilization, soluble transferrin receptor (sTR) levels and ratio of sTR/log ferritin increased significantly in testosterone-treated men. Hormonal and hematologic responses were similar in anemic participants. The majority of testosterone-treated anemic participants increased their hemoglobin into normal range.
CONCLUSIONS:Testosterone-
11) http://www.ncbi.nlm.nih.gov/
J Clin Endocrinol Metab. 2008 Mar;93(3):914-9. Epub 2007 Dec 26.
Effects of graded doses of testosterone on erythropoiesis in healthy young and older men. Coviello AD, Kaplan B, Lakshman KM, Chen T, Singh AB, Bhasin S.
Erythrocytosis is a dose-limiting adverse effect of testosterone therapy, especially in older men.
OBJECTIVE:Our objective was to compare the dose-related changes in hemoglobin and hematocrit in young and older men and determine whether age-related differences in erythropoietic response to testosterone can be explained by changes in erythropoietin and soluble transferrin receptor (sTfR) levels.
DESIGN:We conducted a secondary analysis of data from a testosterone dose-response study in young and older men who received long-acting GnRH agonist monthly plus one of five weekly doses of testosterone enanthate (25, 50, 125, 300, or 600 mg im) for 20 wk.
SETTING:The study took place at a General Clinical Research Center.
PARTICIPANTS:Participants included 60 older men aged 60-75 yr and 61 young men aged 19-35 yr.
OUTCOME MEASURES:Outcome measures included hematocrit and hemoglobin and serum erythropoietin and sTfR levels.
RESULTS:Hemoglobin and hematocrit increased significantly in a linear, dose-dependent fashion in both young and older men in response to graded doses of testosterone (P<0.0001). The increases in hemoglobin and hematocrit were significantly greater in older than young men. There was no significant difference in percent change from baseline in erythropoietin or sTfR levels across groups in either young or older men. Changes in erythropoietin or sTfR levels were not significantly correlated with changes in total or free testosterone levels.
CONCLUSIONS:Testosterone has a dose-dependent stimulatory effect on erythropoiesis in men that is more pronounced in older men. The testosterone-induced rise in hemoglobin and hematocrit and age-related differences in response to testosterone therapy may be mediated by factors other than erythropoietin and sTfR.
——————————
Early MI in Young Male: Testing protocol
lipoprotein(a), homocysteine, antiphospholipid antibodies, plasminogen activator inhibitor-1, factor V Leiden mutation, prothrombin variant, and 5,10-methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism
12) http://www.ncbi.nlm.nih.gov/
J Vasc Surg. 2005 Feb;41(2):255-60.
Thrombophilic risk factors for symptomatic peripheral arterial disease.
Sofi F, Lari B, Rogolino A, Marcucci R, Pratesi G, Dorigo W, Pratesi C, Gensini GF, Abbate R, Prisco D.
Author information
Peripheral arterial disease (PAD) is a common manifestation of systemic atherosclerosis. Over the last years, several novel mediators relevant to the process of atherogenesis have been identified, but few and conflicting data are available on the possible association with PAD symptoms. The aim of this study was to determine an extended thrombophilic risk profile of patients with symptomatic PAD.
METHODS: Two hundred eighty patients with symptomatic PAD admitted to the Department of Vascular Surgery of the University of Florence were compared with 280 control subjects without PAD, matched for age and gender. The following metabolic and genetic risk factors were evaluated: lipoprotein(a), homocysteine, antiphospholipid antibodies, plasminogen activator inhibitor-1, factor V Leiden mutation, prothrombin variant, and 5,10-methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism.
RESULTS: Multivariate logistic regression analysis, adjusted for traditional cardiovascular risk factors, showed a significant association between PAD symptoms and prothrombin variant, altered levels of homocysteine, lipoprotein(a), plasminogen activator inhibitor-1, and antiphospholipid antibodies. Moreover, the presence of high levels of lipoprotein(a) and another metabolic risk factor raised the likelihood of PAD symptoms (dyslipidemia and elevated lipoprotein[a]: odds ratio [OR], 29; 95% confidence interval [CI], 6.2 to 136.2; P <.0001; hyperhomocysteinemia and elevated lipoprotein[a]: OR, 37.7; 95% CI, 3.7 to 381.5; P <.0001). A significant correlation between the number of altered thrombophilic parameters and the Fontaine stage was observed ( R = 0.16; P = .006).
CONCLUSION: There is an independent association between altered levels of important thrombophilic risk factors and PAD symptoms. The clinical significance of this association needs to be tested in prospective population-based trials.
13) http://www.ncbi.nlm.nih.gov/
http://www.ncbi.nlm.nih.gov/
Heart. 2006 Mar;92(3):377-81. Epub 2005 Jul 1.
PAI-1 and homocysteine, but not lipoprotein (a) and thrombophilic polymorphisms, are independently associated with the occurrence of major adverse cardiac events after successful coronary stenting.
Marcucci R, Brogi D, Sofi F, Giglioli C, Valente S, Liotta AA, Lenti M, Gori AM, Prisco D, Abbate R, Gensini GF.
To evaluate the role of factor V Leiden, prothrombin G20210A polymorphism, plasminogen activator inhibitor type 1 (PAI-1) 4G/5G polymorphism, PAI-1, homocysteine, and lipoprotein (a) (Lp(a)) in the occurrence of major adverse cardiac events (MACE) in patients with acute coronary syndromes who underwent coronary stenting.
DESIGN: 520 patients (375 men and 145 women) with acute coronary syndromes and 520 age and sex matched controls were enrolled. MACE were recorded for 109 patients. Heterozygosity for factor V Leiden, prothrombin G20210A polymorphism, and 4G/5G polymorphism did not significantly differ between patients with and without MACE. A significantly higher percentage of patients with increased homocysteine (28% v 19%, p < 0.001) and PAI-1 concentrations (25% v 16%, p < 0.001) had MACE with respect to those who did not. In Kaplan-Meier survival analysis, the overall risk of MACE was significantly higher among patients with increased PAI-1 (p = 0.006) and homocysteine concentrations (p = 0.04). Cox regression analysis adjusted for age, sex, traditional cardiovascular risk factors, renal function, systolic left ventricular function, the number of stenosed vessels, and history of percutaneous coronary intervention or coronary artery bypass grafting showed that homocysteine (odds ratio 7.5, 95% confidence interval (CI) 1.1 to 57.7, p < 0.05) and PAI-1 concentrations (odds ratio 5.3, 95% CI 1.2 to 23.8, p < 0.05) within the fifth quintile (with respect to the first) were significant and independent risk factors for the future occurrence of MACE.
CONCLUSIONS: Increased PAI-1 and homocysteine concentrations are independent risk factors for MACE after successful coronary stenting, whereas Lp(a) and thrombophilic polymorphisms are not predictive.
14) http://atvb.ahajournals.org/
http://www.ncbi.nlm.nih.gov/
Arterioscler Thromb Vasc Biol. 1998 Feb;18(2):152-6.
The PAI-1 gene locus 4G/5G polymorphism is associated with a family history of coronary artery disease.
Margaglione M, Cappucci G, Colaizzo D, Giuliani N, Vecchione G, Grandone E, Pennelli O, Di Minno G.
A family history of ischemic events is a major determinant of coronary artery disease (CAD). Plasma levels of plasminogen activator inhibitor 1 (PAI-1) modulate this risk. A deletion/insertion polymorphism within the PAI-1 locus (4G/5G) affects the expression of this gene. We investigated the relationship between the PAI-1 4G/5G polymorphism in 1179 healthy employees of our institution and the occurrence of CAD in their first-degree relatives. A family history of documented ischemic coronary disease was assessed by a modified WHO questionnaire. The PAI-1 4G/5G polymorphism was evaluated by polymerase chain reaction and endonuclease digestion. The group with a first-degree relative who had suffered from a coronary ischemic episode had a higher number of homozygotes for the deleted allele (4G/4G) of the PAI-1 gene compared with subjects without such a family history (odds ratio [OR] = 1.62, 95% confidence interval [CI]=1.17 to 2.25; P=.005). The frequency of the 4G allele was abnormally high as well (OR=1.29, 95% CI=1.04 to 1.60; P=.025). The individuals with a positive family history were older (P<.001) and exhibited a higher body mass index (P=.033) and total cholesterol levels (P<.001) than those without. In a multiple logistic regression analysis, age (P=.006) and PAI-1 4G/4G (P=.024) independently contributed to a family history of coronary heart disease, with 4G/4G carriers exhibiting a more frequent family history of CAD (OR=1.60). The PAI-1 4G/5G polymorphism to some extent thus accounts for the risk of CAD related to a family history for such an event. These findings support the hypothesis that the 4G variant is a transmissible coronary risk factor
15) http://www.ncbi.nlm.nih.gov/
Clinics (Sao Paulo). 2013 Dec;68(12):1502-8. doi: 10.6061/clinics/2013(12)05.
The involvement of multiple thrombogenic and atherogenic markers in premature coronary artery disease.
Mansur AP, Takada JY, Strunz CM, Avakian SD, César LA, Ramires JA.
To examine the association of atherogenic and thrombogenic markers and lymphotoxin-alfa gene mutations with the risk of premature coronary disease.
METHODS: This cross-sectional, case-control, age-adjusted study was conducted in 336 patients with premature coronary disease (<50 years old) and 189 healthy controls. The control subjects had normal clinical, resting, and exercise stress electrocardiographic assessments. The coronary disease group patients had either angiographically documented disease (>50% luminal reduction) or a previous myocardial infarction. The laboratory data evaluated included thrombogenic factors (fibrinogen, protein C, protein S, and antithrombin III), atherogenic factors (glucose and lipid profiles, lipoprotein(a), and apolipoproteins AI and B), and lymphotoxin-alfa mutations. Genetic variability of lymphotoxin-alfa was determined by polymerase chain reaction analysis.
RESULTS: Coronary disease patients exhibited lower concentrations of HDL-cholesterol and higher levels of glucose, lipoprotein(a), and protein S. The frequencies of AA, AG, and GG lymphotoxin-alfa mutation genotypes were 55.0%, 37.6%, and 7.4% for controls and 42.7%, 46.0%, and 11.3% for coronary disease patients (p = 0.02), respectively. Smoking, dyslipidemia, family history, and lipoprotein(a) and lymphotoxin-alfa mutations in men were independent variables associated with coronary disease. The area under the curve (C-statistic) increased from 0.779 to 0.802 (p<0.05) with the inclusion of lipoprotein(a) and lymphotoxin-alfa mutations in the set of conventional risk factors.
CONCLUSIONS: The inclusion of lipoprotein(a) and lymphotoxin-alfa mutations in the set of conventional risk factors showed an additive but small increase in the risk prediction of premature coronary disease.
16) http://www.ncbi.nlm.nih.gov/
Genet Mol Res. 2013 Dec 19;12(4):6895-906. doi: 10.4238/2013.December.19.8.
Effects of ACE polymorphisms and other risk factors on the severity of coronary artery disease. Guney AI, Ergec D, Kirac D, Ozturhan H, Caner M, Koc G, Kaspar C, Ulucan K, Agirbasli M.
Coronary artery disease (CAD) is a multifactorial disease influenced by genetic and environmental factors. Major risk factors of CAD are hypertension, hyperlipidemia, smoking, family history and obesity. Also polymorphisms in the angiotensin-I converting enzyme (ACE) gene can associate with CAD. The relationship between ACE polymorphisms and other risk factors is not well understood in CAD, likely due to the complex interrelation of genetic and environmental risk factors. The aim of this study was to investigate the associations of CAD risk factors and ACE polymorphisms in patients with CAD. We enrolled 203 consecutive patients and 140 healthy subjects in the study. The severity of CAD was evaluated according to the number of vessels with significant stenosis. ACE insertion (I)/deletion (D) genotype was determined by PCR. The frequency of the DD genotype was significantly higher in patients. D allele frequency was higher among CAD subjects when compared to the control group. The number of stenotic vessels were found to be statistically associated with a high frequency of DD polymorphism and D allele and a low frequency of I allele in patients, especially in male patients. The control group displayed II and ID genotypes more frequently than did the patients. The ACE I/D genotype was associated with hyperlipidemia and smoking history. We consider that the DD polymorphism and D allele may affect the severity of CAD, while I allele may have a protective effect. In conclusion, the ACE I/D genotype may interact with conventional risk criteria in determining the risk of CAD.
17) http://www.ncbi.nlm.nih.gov/
Cardiol J. 2014 Feb 14. doi: 10.5603/CJ.a2013.0107. [Epub ahead of print]
Prognostic value of ACE I/D, AT1R A1166C, PAI-I 4G/5G and GPIIIa a1/a2 polymorphisms in myocardial infarction.
Martínez-Quintana E, Chirino R, Nieto-Lago V, Pérez-Jiménez P, López-Ríos L, Rodríguez-González F.
Coronary artery disease has turned into a prevalent cause of morbymortality contributing some polymorphisms in the recurrence of major adverse cardiac events (MACE).
METHODS: 356 patients with a first myocardial infarction were followed up during a 60 months period to find out if ACE I/D, AT1R A1166C, PAI-I 4G/5G and GPIIIa a1/a2 polymorphisms, in combination with other classical cardiovascular risk factors, can contribute to the relapse of a MACE.
RESULTS: 285 (80.1%) men and 71 (19.9%) women were followed up after a first myocardial infarction. The primary clinical end point, a composite of MACE, was reached in 106 (29.8%) patients. In the Cox univariate survival analysis those risk factors influencing a poorer prognosis were age (p=0.004), a positive family history of coronary artery disease (p=0.007), diabetes (p=0.004), smoking (p=0.024), fibrinolytic therapy (p=0.012) and having 2 or 3 vessels coronary artery disease (p=0.046). Cox proportional hazards regression model showed that patients with the DD genotype had a 1,5 increased risk of having an unfavourable outcome when compared with No-DD genotype patients (RR: 1.561;95% CI 1.048-2.326,p=0.028) and that patients with the ACE DD genotype plus the AT1R No-AA genotype, the GpIIIa No-a1a1 genotype or a combination of both, had twice more risk than any other genotype of a MACE in the follow up (RR: 1.978;95% CI 1.286-3.043,p=0.002).
CONCLUSIONS: Patients with the ACE DD genotype plus 1 or 2 unfavorable genotypes, the AT1R No-AA, the GPIIIa No-a1a1 or a combination of both, have twice the risk of a MACE during their clinical follow up.
18) http://www.ncbi.nlm.nih.gov/
Eur Heart J. 2000 Apr;21(8):633-8.
Searching for a better assessment of the individual coronary risk profile. The role of angiotensin-converting enzyme, angiotensin II type 1 receptor and angiotensinogen gene polymorphisms. Fatini C, Abbate R, Pepe G, Battaglini B, Gensini F, Ruggiano G, Gensini GF, Guazzelli R.
Polymorphisms within renin angiotensin system genes have been investigated as risk factors for coronary artery disease in different populations with contradicting results. The aim of this study was to investigate the genotype distribution and the allele frequencies of ACE, AT1R and AGT gene polymorphisms as coronary artery disease factors and their synergistic effects on coronary risk in an Italian population. METHODS AND RESULTDS: In this study ACE, AT1R and AGT gene polymorphisms were investigated in 205 consecutive coronary artery disease patients and in 209 controls. These polymorphisms were analysed by polymerase chain reaction (PCR) and restriction fragment length polymorphism (RFLP). The ACE D and AGT 235T allele, but not AT1R C allele, frequency was statistically significant in patients. An association between coronary artery disease and ACE DD, AT1R CC and AGT TT genotype, was found by univariate analysis (OR 2.06 P=0.0007, OR 2.49 P=0.009, OR 1.87 P=0. 019, respectively). At multivariate analysis ACE DD and AT1R CC genotype (OR 1.81 P=0.011, OR 2.61 P=0.011, respectively) remained associated with coronary heart disease. Subjects carrying the ACE DD genotype and AT1R C allele showed a stronger association with myocardial infarction (OR=4.02, P<0.0001).
CONCLUSION: Our report indicates the increased risk of coronary artery disease in the presence of ACE DD and AT1R CC genotypes independent of other risk factors, in Italian patients. The present study stresses the relevance of screening for genetic risk factors.
==============================
Quest LAB
Angiotensin Converting Enzyme (ACE) Polymorphism (Insertion/Deletion)
Test Code 11210 CPT Code(s) 81400
5 mL whole blood collected in an EDTA (lavender-top) tube
Protein C and S Activity with Reflex to Protein C and/or S Antigen
Test Code 7942 CPT Code(s) 85303, 85306
If Protein C Activity is <70%, Protein C Antigen is performed at an additional charge (CPT code(s): 85302). If Protein S Activity is <70% for males or <60% for females, Protein S Antigen is performed at an additional charge (CPT code(s): 85305).
Preferred Specimen(s) 4 mL (2 mL in two separate tubes) platelet poor 3.2% sodium citrate plasma collected in (light blue-top) tubes
Thrombophilia Mutation Analysis with Reflex to HR2 Mutation Analysis
CPT Code(s) 81240, 81241 Physician Attestation of Informed Consent
Factor V (Leiden) Mutation Analysis with Reflex to HR2 Mutation Analysis; Prothrombin (Factor II) 20210G >A Mutation Analysis
If Factor V Leiden Mutation Analysis is positive, HR2 Mutation Analysis will be performed at an additional charge (CPT code(s): 81400).
Cardio IQ™ Lipoprotein (a)
Test Code 91729 CPT Code(s) 83695 Preferred Specimen(s) 1 mL frozen serum Minimum Volume 0.5 mL
Cardio IQ Homocysteine
Link to this article:http://wp.me/p3gFbV-1he
Jeffrey Dach MD
7450 Griffin Road, Suite 190
Davie, Fl 33314
954-792-4663
www.jeffreydach.com
www.drdach.com
www.naturalmedicine101.com
www.bioidenticalhormones101.com
www.truemedmd.com
Click Here for: Dr Dach’s Online Store for Pure Encapsulations Supplements
Click Here for: Dr Dach’s Online Store for Nature’s Sunshine Supplements
Web Site and Discussion Board Links:
jdach1.typepad.com/blog/
disc.yourwebapps.com/Indices/244124.html
disc.yourwebapps.com/Indices/244066.html
disc.yourwebapps.com/Indices/244067.html
disc.yourwebapps.com/Indices/244161.html
disc.yourwebapps.com/Indices/244163.html
Disclaimer click here: www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship. Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Copyright (c) 2014 Jeffrey Dach MD All Rights Reserved. This article may be reproduced on the internet without permission, provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.









Testosterone and the Heart - Jeffrey Dach MD February 26, 2014 at 6:51 AM
[…] For part three click here. […]
Mark R. July 14, 2014 at 9:25 AM
Testosterone therapy should be used with caution. Thanks for the information Dr. Dach. I’ve learned a lot through this post. I will be very careful starting now since I am diagnosed with Low-T and my doctor advised me to take testosterone therapy.